Mass migration triggered by the unfolding crisis in Syria has heightened interest in radiology's role in the protection of children. For young unaccompanied persons arriving in Europe without documentation, imaging can be used to determine age and, as a result, their refugee status, having a direct impact on the aid they receive and where they can live.
At the other end of the spectrum of its uses, bone assessment is also a means to gauge the skeletal age of football players in tournaments such as the under-17 and under-20 world cups. This need arises when personal documents are lacking for players who come from countries with no official birth registration systems and when there is a suspicion that an older player is being included in a younger age category.
"This misclassification entails not only physical risk of exposing weaker players to injuries caused by older players but also undermines the system of recognition or economic reward, which may be considerable in some cases," said Dr. Sandra Diaz Ruiz, PhD, pediatric radiologist at the Astrid Lindgren Children's Hospital, part of the Karolinska University Hospital in Stockholm.
Part of the appeal of MRI in young footballers is its lack of ionizing radiation, and the modality has been used in wrist assessments by the International Federation of Association Football (FIFA) since 2003.
MRI is not currently used to assess bone age in routine practice, but Diaz believes that it could be standardized to become an option both in clinical diagnosis of special syndromes and in forensic work, the latter being the main focus of her presentation today. As an adjunct to other methods, MRI yields accurate results to specific questions, but there are pitfalls, and problems can arise from the absence of standards to ensure that the age established by the scientific evidence is correct. Moreover, the fact that research predominantly pertains to males and Caucasians means that it cannot be used as a general reference.
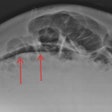
 Measurements taken from knee MRI can help determine age, but protocols and grade scales must be standardized for routine practice in bone maturation assessment. Images courtesy of Dr. Sandra Diaz Ruiz, PhD.
Measurements taken from knee MRI can help determine age, but protocols and grade scales must be standardized for routine practice in bone maturation assessment. Images courtesy of Dr. Sandra Diaz Ruiz, PhD."There are not enough studies that represent the entire population. Instead small studies aim to answer specific questions," she told ECR Today. "Furthermore, some involve several grade scales of the same body part examined with different MR field strengths. The interpretation of these grade scales may be confusing to inexperienced radiologists."
She pointed to other studies which found that because MRI is a lengthy process and sensitive to body movement, this is a significant limitation of its use children.
Other factors in bone age estimation remain controversial: gender, ethnicity, nutrition, physical activity, geographical location, other socioeconomic factors, and exposure to the sun as an acceleration factor in maturation should all be considered. Widening study cohorts to include a range of different groups of subjects could also be looked at and would constitute a way of reaching consensus on protocols and grade scales. These studies must be wide, multicenter and guarantee the inclusion of these different factors, according to Diaz.
Beyond determining age in football and forensic medicine, a key application of bone age assessment is the evaluation of growth and puberty disorders. Dr. Fabrice Dedouit, PhD, head of the imaging and forensic anthropology unit of the University Center of Legal Medicine in Lausanne-Geneva, Switzerland, thinks such evaluation is fundamental to determining patient management and choice of therapy.
"In patient follow-up it is critical to continue using the same method and not change to a different means of assessment," he said.
The two most widely used systems are the Greulich and Pyle Atlas (GP) and the Tanner Whitehouse (TW) methods. Published in 1959, GP is the most widely used. It is based on hand x-rays from 1,000 Americans of northern European descent living in Ohio, between 0 years and 18 years in, which were taken from the Brush Foundation longitudinal study between 1931 and 1942 and compiled into an atlas. To help determine bone age, plain x-rays of the left hand and wrist can be compared with reference atlas images for each age category and both sexes.
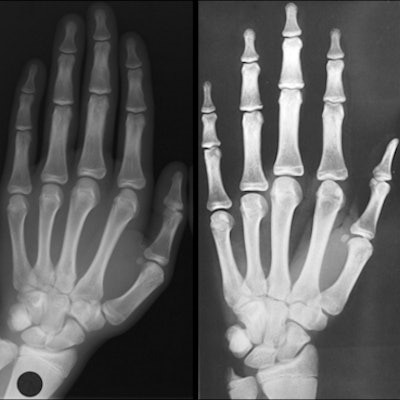
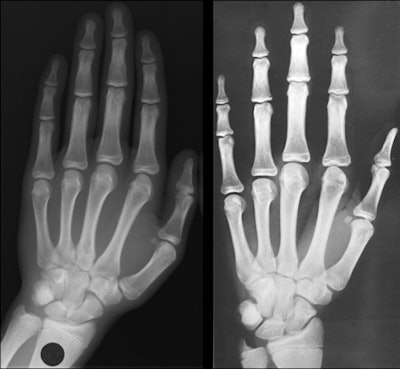 Left: Clinical x-ray of a young male with a chronological age of 16 years and 4 months. Right The closest image in the Greulich and Pyle Atlas is the male standard number 28 corresponding to a skeletal age of 16 years old. A limitation of bone maturation assessment using GP atlas images is that similarity can only help determine skeletal age, not chronological age. Images courtesy of Dr. Fabrice Dedouit, PhD.
Left: Clinical x-ray of a young male with a chronological age of 16 years and 4 months. Right The closest image in the Greulich and Pyle Atlas is the male standard number 28 corresponding to a skeletal age of 16 years old. A limitation of bone maturation assessment using GP atlas images is that similarity can only help determine skeletal age, not chronological age. Images courtesy of Dr. Fabrice Dedouit, PhD.Evaluation is based on the existence and morphology of the epiphyses of the metacarpals and the phalanges and their fusion, the carpal bones, and the inferior epiphyseal points of the ulna and radius. While it is simple, with low inter- and intraobserver differences, critics state that the method is based on an old study and is not representative of modern, multiethnic, taller, and heavier populations from various socioeconomic backgrounds.
The Tanner Whitehouse method, based on data compiled in 1962 from British children born between 1940 and 1955, involves the assignment of a score to each of the ossification centers, involving 20 bones, visible in the x-ray. The development of each bone within the hand/wrist complex is divided into a series of stages from A (initial radiological aspect) to H (final mature radiological aspect), when the bone has achieved full adult morphology. Each bone is assessed individually for stage, with each stage assigned a numeric score. All numeric scores are then added together to achieve a cumulative score, which is then related to a chronological age.
The method was updated with data from Scotland in 1975 (TW2) and then again in 2001 (TW3) with data from Europe, Argentina, Japan, and the U.S. However, it is time-consuming, difficult to learn, involves arbitrary assignment of scores to the degrees of maturity, and only gives a rough staging of ossification of the ulna and radius, according to Dedouit.
Bone age assessment has a key role in the confirmation of normal variants of growth, interpretation of hormone blood levels in children during puberty, and diagnosis of precocious puberty and hyperandrogenism, such as congenital adrenal hyperplasia characterized by advanced bone age. Assessment is also pivotal in the decision whether to treat children with precocious puberty and congenital adrenal hyperplasia, in monitoring skeletal response to the treatment, and also defining the right moment to start replacement treatment in children with hypogonadism. Evaluating children with growth retardation and advanced or delayed puberty and monitoring pediatric patients being treated with growth hormone replacement therapy are two other areas that rely on bone age assessment.
"Radiological results of bone age must always be combined with clinical evaluation and paraclinic results -- hormonological if necessary -- to explore and assess the pathologies or to help determine chronological age," he noted.
Originally published in ECR Today on 1 March 2017.
Copyright © 2017 European Society of Radiology