4D flow MRI has revealed impaired cardiac blood flow in patients with chronic obstructive pulmonary disease (COPD), according to a May 12 presentation at at the International Society for Magnetic Resonance in Medicine (ISMRM) annual meeting in Honolulu, HI.
The finding is from an initial analysis of 256 participants in a clinical trial and reinforces emerging evidence of complex cardiopulmonary hemodynamic interactions in COPD, noted researcher David Dushfunian, MD, of Northwestern University in Chicago.
“We propose 4D flow MRI as a noninvasive method to study heart-lung interactions, which may also aid in evaluating outcomes and progression in COPD,” Dushfunian said.
COPD prevalence and associated mortality rates due to heart failure have increased over the past decades. Previous studies have shown that left ventricular filling is impaired in patients with COPD and thus further investigations are essential for understanding the COPD-heart failure relationship, Dushfunian explained.
To that end, Dushfunian and colleagues used 3D time-resolved phase contrast imaging (4D flow MRI) to characterize associations between physiologic metrics and COPD subtypes with key right heart hemodynamic parameters: blood flow velocity, stasis, viscous energy loss, and kinetic energy in the right atrium, right ventricle, and main pulmonary artery.
The group performed a preliminary imaging analysis of 256 patients enrolled in a multicenter, longitudinal case-control study of COPD cases with 20-plus pack years of smoking and controls. Data were acquired on both Siemens Healthineers and GE HealthCare MRI systems, with all datasets processed for background phase correction, noise masking, and velocity anti-aliasing, following established guidelines and algorithms, Dushfunian noted.
According to the analysis, there were significant correlations between the tested parameters in each heart structure and COPD subtypes. These included senile, obstructive and restrictive chronic pulmonary fibrosis emphysema, vanish, and combined bronchitic-apical emphysema.
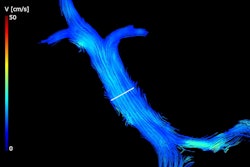
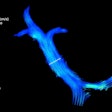
 Examples of hemodynamic parameter maps superimposed on their corresponding anatomic data for two participants. Participant A represents an example of good flow with lower right ventricle stasis, increased right atrium kinetic energy, and increased mean velocity when compared to the sample’s average calculations. Opposite findings are highlighted by the visualizations of participant B representing an example of poor flow.David Dushfunian, MD, and ISMRM
Examples of hemodynamic parameter maps superimposed on their corresponding anatomic data for two participants. Participant A represents an example of good flow with lower right ventricle stasis, increased right atrium kinetic energy, and increased mean velocity when compared to the sample’s average calculations. Opposite findings are highlighted by the visualizations of participant B representing an example of poor flow.David Dushfunian, MD, and ISMRM
Specifically, the extent of patients’ lung damage was positively associated with peak velocity of blood flow (velocity max) in the right atrium (r = 0.2, p < 0.01) and right ventricle (r = 0.24, p < 0.01). Meanwhile, total lung volume was inversely correlated with right atrium kinetic energy (r = -0.17, p = 0.01) as well as right ventricle kinetic energy (r = -0.20, p < 0.01) and viscous energy loss (r = -0.16, p = 0.02).
In addition, airway thickness was significantly correlated with kinetic energy and viscous energy loss in the right atrium, right ventricle, and main pulmonary artery (r = 0.19-0.32, p < 0.01), according to the findings.
“We present the potential of 4D flow MRI to noninvasively assess the cardiopulmonary hemodynamic interaction in COPD, which may allow early detection and management of subclinical heart failure secondary to COPD,” Dushfunian said.
Ultimately, the results reinforce emerging evidence of complex cardiopulmonary hemodynamic interactions in COPD, with previous findings showing vascular remodeling in COPD linked to reduced left ventricular filling, stroke volume, and cardiac output, Dushfunian said.
“Future directions include assessing inter-vendor variations in hemodynamic quantification as well as employing 5D flow to examine how varying respiratory patterns in COPD impact cardiac hemodynamics,” he concluded.
Check out AuntMinnie’s full coverage of ISMRM 2025 here.