The spread of Hepatitis C has created a severe shortage of cadaver liver donors, leaving doctors little choice but to transplant entire right lobes from living donors. In an award-winning study presented in Monday's gastrointestinal sessions at RSNA, Dr. Ihab Kamel from Beth Israel Deaconess Medical Center in Boston showed how transplantation leads to consistent and predictable regeneration patterns in both donors and recipients. The knowledge will help doctors understand what's normal, and alert them to potential problems following right-lobe transplantation.
"Our objective was to document specific patterns of segmental regeneration and vascular growth in both donors and recipients after living-donor liver transplantation," Kamel said. "If we can define specific patterns, then deviation from these patterns would suggest complication, and may warrant further evaluation."
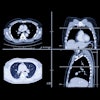
In the study, 10 donors and eight recipients ages 20-56 underwent both pre- and postoperative multidetector-row CT scanning (LightSpeed QX/i, GE Medical Systems, Waukesha, WI) following administration of oral and IV contrast using 180 mL of Optiray (Mallinckrodt, Hazelwood, MO) at 5 mL/sec. Arterial-phase images were acquired at 18 seconds, with 1.25 mm collimation, table speed of 7.5; and portal venous images were acquired at 60 seconds, with 2.55-mm slice thickness and table speed 15, according to the Kamel.
Postoperative scans were performed when clinically necessary, so the follow-up time varied between eight days and 14 months, Kamel said. There were 29 postoperative scans in all.
The resulting axial images were postprocessed on a GE Advantage workstation, and all scans were evaluated for changes in segmental liver volume, as well as for vascular supply regeneration patterns, using maximum intensity projection and multiplanar volume rendering to evaluate the parenchyma and vascularity.
"We performed [hand] tracing to determine organ volume relative to the change in volume of the liver and spleen over time following transplantation," Kamel said.
The images showed that liver regeneration began immediately after transplantation in both donors and recipients. However, the initial rate of volumetric increase was greater in recipients (94% of postoperative volume) than in donors (34%). At 30 and 60 days after surgery, the volumetric increases for donors were 34% and 66% respectively; for recipients the growth was 80% and 114% respectively. Recipients' liver volumes doubled in 4-6 weeks, as compared with an average increase of 66% in donors, followed by a gradual plateau for both groups.
"In recipients the growth is faster and reaches a higher peak, in about two months, as compared to a more gradual increase in donors which peaked in about six months," Kamel said.
Liver vascularity also grew along with the healthy parenchyma, but not evenly between patient groups. While donors' increased blood supply came mainly from the left portal vein, recipients developed new capsular collateral vessels, and received blood from the right portal vein. The spleens of donors and recipients also reacted differently to the surgery, Kamel said.
"When we looked at relative changes in splenic volume over time (in donors), we noticed an immediate increase in volume probably related to a decrease in portal pressure following resection," he said. "What was unexpected is that the initial increase in donor spleen volume plateaus over several months, then gradually [returns] to normal, probably related to an increase in portal pressure following liver resection."
In summary, liver volume immediately increases in both donors and recipients, but the increase is faster and reaches a higher peak in recipients, Kamel said. "In splenic volume, expect an initial increase in donors, however, a decrease in recipients. Both donors and recipients will have developed collateral channels on follow-up CT. Documenting these patterns ensures greater survival and positive outcomes, and deviation from these patterns warrants further investigation," he said.
Session chair Dr. Richard Baron from the University of Pittsburgh presented Kamel with an RSNA award for best subspecialty study (gastrointestinal) by a fellow. Kamel said the next step in his team's efforts might be to correlate regeneration patterns with long-term clinical outcomes.
By Eric BarnesAuntMinnie.com staff writer
November 28, 2000
Copyright © 2000 AuntMinnie.com
Click here to view the rest of AuntMinnie’s coverage of the 2000 RSNA conference.
Click here to post your comments about this story.