CHICAGO – Ultrafast CT angiography does an excellent job of assessing coronary artery disease, as long as its limitations are kept in mind. A presenter at Tuesday’s cardiac scientific sessions at RSNA quantified the modality’s performance in vessel visibility, detection of atherosclerosis, and stenosis.
According to Dr. Christophe Herzog of the University of Frankfurt in Germany, the modality performs best in proximal heart segments, heart rates lower than 70 beats per minute, and in vessels larger than 1.5 mm in diameter.
“The purpose of our study was to evaluate the performance and limitations of CT angiography regarding the detection of coronary atherosclerosis, the quantification of high-grade stenosis higher than 50%, and the overall visibility of the coronary arteries,” Herzog said.
The group examined 62 patients including 37 men and 25 women with a mean age of 54 years and a mean heartbeat of 63 bpm, between January and September 2000. All patients were examined with conventional angiography and ultrafast CT; 20 patients were also examined with intravascular ultrasound.
Patients underwent CT on a Plus 4 VolumeZoom (Siemens Medical Systems, Erlangen, Germany) multidetector-row scanner, with a pitch of 1, collimation 4 x 1 mm, 140 kV, 300 mA, 500 ms rotation time, start delay 35 seconds with a test bolus of 30 mL of contrast material, according to Herzog.
The resulting data sets were reconstructed in three ways: as axial scans, as 3-D volume-rendered objects using retrospective ECG gating, and as orthogonal multiplanar reconstructions (MPRs).
“All measurements were done using the American Heart Association classifications for coronary artery sequences,” Herzog said. “Each sequence was evaluated independently by two radiologists and once cardiologist. After that we chose three groups using proximal, medial and distal sequences. The measure parameters were vascular diameter, [heartbeat] frequency, the visibility of vessels, and the amount of high-grade stenosis,” Herzog said.
Because the temporal resolution was 250 msec, the best results were obtained in patients with heart rates below 60 bpm. For these patients there was clear correspondence in detection of vascular pathology between the three reconstruction methods.
“We found that overall visibility for all sequences, for all heartbeat (rates), for all patients was 66.7%,” he said. “The best results were obtained with the proximal sequence: 94.4% visibility. The medial and distal sequences only showed visibility of slightly over 56%. The best results were obtained between 50-60 bpm.”
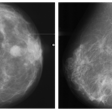
In addition, calcified plaque was detected in 96% of all cases, while the detection of non-calcified plaque varied between 60-80% depending on localization, the reader’s experience, and vessel diameter.
“For the detection of arteriosclerosis, we found that 71.6% of plaque was detected in total. The best results were obtained for the proximal sequence, with a detectability of 85.7%. The best detection rate was obtained in the [right coronary artery}, in 87.2% of total vessels.” Herzog said.
High-grade stenoses were detected with an overall sensitivity of 74.6%, Herzog said. “The best results again were in the proximal vessels, with nearly 89% sensitivity.”
The axial scan measurements were less precise than those enabled by the orthogonal MPRs, which detected noncalcified plaque even in the medial coronary segments in more than 83% of the patients. Yet the total negative predictive value of all ultrafast CT exams was zero.
By Eric Barnes
AuntMinnie.com staff writer
November 29, 2000
According to Dr. Christophe Herzog of the University of Frankfurt in Germany, the modality performs best in proximal heart segments, heart rates lower than 70 beats per minute, and in vessels larger than 1.5 mm in diameter.
“The purpose of our study was to evaluate the performance and limitations of CT angiography regarding the detection of coronary atherosclerosis, the quantification of high-grade stenosis higher than 50%, and the overall visibility of the coronary arteries,” Herzog said.
The group examined 62 patients including 37 men and 25 women with a mean age of 54 years and a mean heartbeat of 63 bpm, between January and September 2000. All patients were examined with conventional angiography and ultrafast CT; 20 patients were also examined with intravascular ultrasound.
Patients underwent CT on a Plus 4 VolumeZoom (Siemens Medical Systems, Erlangen, Germany) multidetector-row scanner, with a pitch of 1, collimation 4 x 1 mm, 140 kV, 300 mA, 500 ms rotation time, start delay 35 seconds with a test bolus of 30 mL of contrast material, according to Herzog.
The resulting data sets were reconstructed in three ways: as axial scans, as 3-D volume-rendered objects using retrospective ECG gating, and as orthogonal multiplanar reconstructions (MPRs).
“All measurements were done using the American Heart Association classifications for coronary artery sequences,” Herzog said. “Each sequence was evaluated independently by two radiologists and once cardiologist. After that we chose three groups using proximal, medial and distal sequences. The measure parameters were vascular diameter, [heartbeat] frequency, the visibility of vessels, and the amount of high-grade stenosis,” Herzog said.
Because the temporal resolution was 250 msec, the best results were obtained in patients with heart rates below 60 bpm. For these patients there was clear correspondence in detection of vascular pathology between the three reconstruction methods.
“We found that overall visibility for all sequences, for all heartbeat (rates), for all patients was 66.7%,” he said. “The best results were obtained with the proximal sequence: 94.4% visibility. The medial and distal sequences only showed visibility of slightly over 56%. The best results were obtained between 50-60 bpm.”
In addition, calcified plaque was detected in 96% of all cases, while the detection of non-calcified plaque varied between 60-80% depending on localization, the reader’s experience, and vessel diameter.
“For the detection of arteriosclerosis, we found that 71.6% of plaque was detected in total. The best results were obtained for the proximal sequence, with a detectability of 85.7%. The best detection rate was obtained in the [right coronary artery}, in 87.2% of total vessels.” Herzog said.
High-grade stenoses were detected with an overall sensitivity of 74.6%, Herzog said. “The best results again were in the proximal vessels, with nearly 89% sensitivity.”
The axial scan measurements were less precise than those enabled by the orthogonal MPRs, which detected noncalcified plaque even in the medial coronary segments in more than 83% of the patients. Yet the total negative predictive value of all ultrafast CT exams was zero.
By Eric Barnes
AuntMinnie.com staff writer
November 29, 2000
Copyright © 2000 AuntMinnie.com
Click here to view the rest of AuntMinnie’s coverage of the 2000 RSNA conference.
Click here to post your comments about this story.