As with the rest of radiology, women's imaging in 2020 has been marked by the COVID-19 pandemic, which has resulted in drastic drops in imaging volume. At the same time, nagging questions persist about whether mammography screening exams postponed due to COVID-19 could result in higher breast cancer rates later on.
But researchers and readers have also discovered hopeful stories in women's imaging in 2020, including improvements in MRI and an assurance in the benefits of breast screening programs.
Before the pandemic swept the news cycle, 2020 was supposed to be a big year for breast density notification laws, as there has been continued discussion about implementing federal notification regulations and whether state laws reliably improve access to supplemental screening.
Instead, researchers and readers appear to have doubled down on questioning established principles. With norms and expectations thrown out of whack, it's no wonder we're reevaluating what used to be day-to-day practices.
For breast imagers, this has led to questioning whether screening mammography still makes sense (it does) or if there's a way to improve MRI for breast imaging (there is). However, questions around breast screening and the use of MRI pale in comparison with the paramount topic of the year: the COVID-19 pandemic.
Women's imaging upended by the pandemic
It's hard to overstate the effects of COVID-19 on the entire continuum of care for women's imaging in 2020. From screening to diagnosis to breast cancer treatment, facilities have learned to cope with massive declines in imaging volume and contend with providing quality care while keeping patients and staff safe.
An April survey from market research firm IMV Medical Information Division, a sister company of AuntMinnie.com, showed just how much of an impact the pandemic has had on women's imaging from the start. X-ray mammography units experienced an astounding 70.4% decline in procedure volume early in the year -- a drop much higher than the second-most affected modality, fixed radiographic fluoroscopy systems, which experienced a 48.1% decline in volume.
| Impact on procedure volume due to novel coronavirus in U.S. | |
| Imaging modality | Procedure volume |
| Mobile general x-ray units | -6.8% |
| Fixed PET and/or PET/CT | -24.5% |
| CT scanners | -37.5% |
| Fixed general x-ray radiography units | -38.6% |
| Fixed C-arm systems | -40.1% |
| Ultrasound units | -42.7% |
| Portable C-arm units | -44.6% |
| Fixed nuclear medicine cameras | -47% |
| Fixed MRI scanners | -47.4% |
| Fixed radiographic fluoroscopy systems | -48.1% |
| X-ray mammography units | -70.4% |
The pandemic also resulted in breast imaging facilities getting creative to keep things running as smoothly as possible. In April, breast imaging chairs from across the U.S. shared how they're triaging patients and managing workflows in an uncertain time.
The changes implemented included temporarily stopping routine mammography and ultrasound screenings -- a factor that likely contributed to the reported drop in procedure volume. The institutions also adopted stricter infection control policies, such as implementing social distancing in waiting areas, requiring staff and patients to wear masks, and limiting the number of appointments per day.
As the pandemic has continued, women's imaging leaders are now asking new questions. Namely, how will delays in screening and treatment ultimately affect breast cancer outcomes? It's possible some of the discussion at RSNA 2020 will focus on this very topic.
It's still too early to give a definitive answer on the long-term effects of the pandemic for patients or facilities. However, even back in April, Dr. Jennifer Harvey from the University of Rochester Medical Center was optimistic that at least some of the key learnings will be positive.
"I'm hopeful this crisis will build collaboration between our subspecialty divisions and our community and regional sites," she wrote. "We can all be stronger for going through this together."
Big questions around screening mammography
Screening mammography may be a half-century old, but it has been a surprisingly hot women's imaging topic this year. Readers and researchers want to know whether programs designed to reduce late-stage breast cancer diagnoses are still beneficial in 2020. The answer appears to be a resounding yes.
Mammography screening reduced the risk of dying of breast cancer by 41% within 10 years of diagnosis, according to the findings of one May study that included nearly one-third of the screening-eligible population in Sweden. The study also found a 25% reduction in advanced breast cancer incidence among women who used screening mammography compared with those who did not.
One of the researchers behind that study was Dr. László Tabár, a Swedish radiologist and oncologist known worldwide as the "father" of mammography screening. In a well-received interview with AuntMinnie.com, Tabár said studies like the one above are important for reassuring physicians that screening is the best way to reduce the risk of premature death from breast cancer.
"Breast cancer is a terrible disease and it kills too many women, but by carrying out these very demanding and complex studies, it has been proved that early detection combined with efficient treatment can significantly reduce mortality from the disease," he said.
Despite the consensus that breast screening saves lives, debate still swirls regarding the ideal ages and frequency with which to conduct routine mammography. This is partially because breast cancer screening programs are expensive to run, especially in the U.S.
A JAMA Internal Medicine study found that the total cost of annual breast cancer screening for commercially insured women younger than age 50 was $2.1 billion -- an astounding sum that made the research team question the cost-effectiveness of screening younger women.
"These costs are borne despite the unclear trade-off between clinical benefits and risks of screening women aged 40 through 49 years," the authors wrote in the article.
| Annual breast cancer screening among women 40-49 with commercial insurance | ||
| Exams | Mean cost per beneficiary screened | Total national cost |
| Screening mammography | $249 | $1.5 billion |
| Recall | $56 | $337 million |
| Other diagnostic tests | $45 | $273 million |
| Total screening and evaluation | $353 | $2.1 billion |
In a similar study, a Harvard-led research team calculated whether it is cost-effective to perform screening mammography in healthy older women. In the resulting Annals of Internal Medicine study, the team found breast cancer deaths were not substantially reduced for Medicare beneficiaries older than 75 who continued annual mammography, compared with those who did not.
But in a critique of that study, clinicians at Johns Hopkins said the research didn't include data of women screened with newer and better screening technologies, including digital breast tomosynthesis (DBT). Like its technological predecessors, DBT allows clinicians to detect cancer early. But the novel ability made possible by DBT to view slides in three dimensions has helped breast imagers in 2020 find more cancers with fewer recalls.
DBT's strength for cancer detection was perhaps most apparent in a February Journal of the American College of Radiology study that found the screening modality identified more than twice as many cancers as full-field digital mammography (FFDM) alone or as a combination of DBT and FFDM.
Hopeful promise of MRI for breast imaging
As the year went on, and perhaps as news of the COVID-19 pandemic grew dispiriting, women's imagers turned their attention to a topic a little more hopeful -- MRI for breast imaging. While the use of MRI for screening and diagnostic imaging has been a popular topic for most of the year, MRI news really picked up in the summer and fall.
In August, researchers detailed some of the advances making MRI quicker, more accurate, and less costly for breast screening at the Society for MR Radiographers & Technologists annual meeting. One of the more promising advancements discussed was the use of abbreviated protocols that can cut down scan time to mere minutes.
In fact, one study showed a 10-minute MRI scan found more than twice the number of invasive cancers in women with dense tissue than DBT. The same research team is now investigating whether abbreviated MRI screening could be cost-effective and still accurate if conducted every two to three years.
Another big MRI topic in 2020 is the use of diffusion-weighted imaging (DWI), a way to perform contrast-free MRI. Getting rid of gadolinium could be a huge win for women's imaging, since it would not only cut down on appointment time but also reduce concerns regarding the contrast agent's safety.
The future of DWI-MRI for breast imaging may not be far off, either. In May, researchers detailed how they repurposed a DWI-MRI protocol originally designed for brain imaging. The multiplexed sensitivity-encoding (MUSE) protocol resulted in better image quality and improved signal-to-noise ratio for breast lesions.
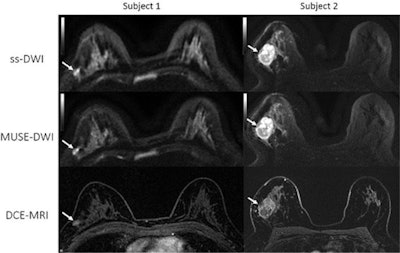 Comparison of single-shot (ss) DWI, MUSE DWI, and dynamic contrasted-enhanced (DCE) MRI axial images for two patients with biopsy-proven invasive ductal carcinoma. Image courtesy of the RSNA.
Comparison of single-shot (ss) DWI, MUSE DWI, and dynamic contrasted-enhanced (DCE) MRI axial images for two patients with biopsy-proven invasive ductal carcinoma. Image courtesy of the RSNA."MUSE DWI yielded significantly improved image quality compared with single-shot DWI in phantoms and participants," the team wrote.
In 2020, researchers also demonstrated the potential of MRI to improve breast cancer care. A March study found patients with breast cancer who underwent presurgical MRI had fewer positive surgical margins and repeat surgeries than those who did not. The study highlighted that MRI can have big breast imaging benefits -- even with longer scan times and the need for gadolinium.
All of these studies point to MRI being a surprisingly bright spot in an otherwise dark year for women's imaging. It's almost certain that researchers at RSNA 2020 will continue to share advances making MRI even better, giving breast images another tool in their arsenal to identify cancer early and ultimately save lives.