J Natl Cancer Inst 2001 Apr 18;93(8):630-5
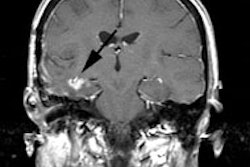
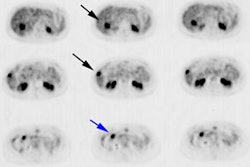
Axillary lymph node staging in breast cancer by
2-fluoro-2-deoxy-D-glucose-positron emission tomography: clinical evaluation and
alternative management.
Greco M, Crippa F, Agresti R, Seregni E, Gerali A, Giovanazzi R, Micheli A,
Asero S, Ferraris C, Gennaro M, Bombardieri E, Cascinelli N.
BACKGROUND: Surgical removal of axillary lymph node and histologic examination
for metastases are used to determine whether adjuvant treatment is necessary for
patients with breast cancer. Axillary lymph node dissection (ALND) is a costly
procedure associated with various side effects, and 80% or more of patients with
tumors of 20 mm or less are lymph node negative and might avoid ALND. In this
study, we evaluated whether an alternative, noninvasive method--i.e., positron
emission tomography (PET) with 2-[(18)F]fluoro-2-deoxy-D-glucose (FDG)-- could
be used to determine axillary lymph node status in patients with breast cancer.
METHODS: One hundred sixty-seven consecutive patients with breast cancers of 50
mm or less (range = 5-50 mm; mean = 21 mm) scheduled for complete ALND were
studied preoperatively with FDG-PET, and then PET and pathology results from
ALND were compared. All statistical tests were two-sided. RESULTS: The overall
sensitivity, specificity, and accuracy of lymph node staging with PET were 94.4%
(PET detected 68 of 72 patients with axillary involvement; 95% confidence
interval [CI] = 86.0% to 98.2%), 86.3% (82 of 95 patients without axillary
involvement; 95% CI = 77.8% to 91.9%), and 89.8% (150 of 167 patients with
breast cancer; 95% CI = 84.2% to 93.6%), respectively. Positive- and
negative-predictive values were 84.0% (68 patients with histologically positive
lymph nodes of 81 patients with positive FDG-PET scan; 95% CI = 74.2% to 90.5%)
and 95.3% (82 patients with histologically negative lymph nodes of 86 patients
with negative FDG-PET scan; 95% CI = 88.2% to 98.5%), respectively. When PET
results for axillary metastasis were analyzed by tumor size, the diagnostic
accuracy was similar for all groups (86.0%-94.2%), with higher sensitivity for
tumors of 21-50 mm (98.0%) and higher specificity for tumors of 10 mm or less
(87.8%), and the range was 93.5%-97.3% for negative-predictive values and
54.5%-94.1% for positive-predictive values. Among the 72 patients with axillary
involvement, PET detected three or fewer metastatic lymph nodes in 27 (37.5%)
patients, about 80% of whom had no clinically palpable axillary lymph nodes.
CONCLUSIONS: Noninvasive FDG-PET appears to be an accurate technique to predict
axillary status in patients with breast cancer and thus to identify patients who
might avoid ALND. These results should be confirmed in large multicenter
studies.