JAMA 2001 Nov 7;286(17):2120-7
Positron emission tomography in evaluation of dementia: Regional brain
metabolism and long-term outcome.
Silverman DH, Small GW, Chang CY, Lu CS, Kung De Aburto MA, Chen W, Czernin J,
Rapoport SI, Pietrini P, Alexander GE, Schapiro MB, Jagust WJ, Hoffman JM,
Welsh-Bohmer KA, Alavi A, Clark CM, Salmon E, de Leon MJ, Mielke R, Cummings JL,
Kowell AP, Gambhir SS, Hoh CK, Phelps ME.
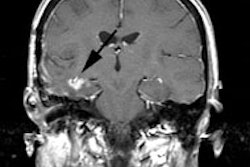
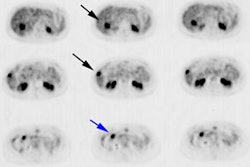
CONTEXT: Deficits in cerebral glucose utilization have been identified in
patients with cognitive dysfunction attributed to various disease processes, but
their prognostic and diagnostic value remains to be defined. OBJECTIVE: To
assess the sensitivity and specificity with which cerebral metabolic patterns at
a single point in time forecast subsequent documentation of progressive
dementia. DESIGN, SETTING, AND PATIENTS: Positron emission tomography (PET)
studies of [(18)F]fluorodeoxyglucose in 146 patients undergoing evaluation for
dementia with at least 2 years' follow-up for disease progression at the
University of California, Los Angeles, from 1991 to 2000, and PET studies in 138
patients undergoing evaluation for dementia at an international consortium of
facilities, with histopathological diagnoses an average of 2.9 years later,
conducted from 1984 to 2000. MAIN OUTCOME MEASURES: Regional distribution of
[(18)F]fluorodeoxyglucose in each patient, classified by criteria established a
priori as positive or negative for presence of a progressive neurodegenerative
disease in general and of Alzheimer disease (AD) specifically, compared with
results of longitudinal or neuropathologic analyses. RESULTS: Progressive
dementia was detected by PET with a sensitivity of 93% (191/206) and a
specificity of 76% (59/78). Among patients with neuropathologically based
diagnoses, PET identified patients with AD and patients with any
neurodegenerative disease with a sensitivity of 94% and specificities of 73% and
78%, respectively. The negative likelihood ratio of experiencing a progressive
vs nonprogressive course over the several years following a single negative
brain PET scan was 0.10 (95% confidence interval, 0.06-0.16), and the initial
pattern of cerebral metabolism was significantly associated with the subsequent
course of progression overall (P<.001). CONCLUSION: In patients presenting
with cognitive symptoms of dementia, regional brain metabolism was a sensitive
indicator of AD and of neurodegenerative disease in general. A negative PET scan
indicated that pathologic progression of cognitive impairment during the mean
3-year follow-up was unlikely to occur.