Mucosa Associated Lymphoid Tissue Lymphoma- MALTOMA
Bronchus Associated Lymphoid Tissue Lymphoma- BALTOMA
Previously "Pseudolymphoma"
View cases of MALTOMA/BALTOMA
Clinical:
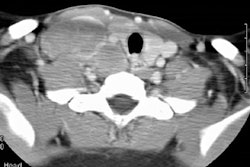
Lymphoid tissue can be found in sites outside of lymph nodes including the oral/pharyngeal mucosa, the gastrointestinal tract (Peyer's patches), and within the lungs (bronchial associated lymphoid tissue). Most lymphomas that involve the lung are disseminated by a systemic process. Primary lymphomas of the lung are rare (less than 1% of lymphomas) extranodal lymphomas that are felt to arise from this bronchus associated lymphoid tissue. Within the lungs, a MALTOMA (also referred to as an extranodal marginal zone mucosa associated lymphoid tissue lymphoma [7]) is characterized by a mass-like infiltrate of atypical lymphoid cells in a primarily peribronchial distribution. MALT lymphoma is felt to result from chronic inflammation of the BALT (bronchus associated lymphoid tissue) [6].At histologic analysis, these lesions are found to be monoclonal proliferations, typically B-cell (T-cells in a small percentage of cases), and should be considered a low-grade non-Hodgkins lymphoma (the lesion is slowly progressive).
The peak age of incidence is in the sixth decade [6]. Patients are usually asymptomatic, but occasionally present with cough, fever, or weight loss [7]. Up to 29% of cases are associated with autoimmune disorders [7]. MALTOMA's may be seen in patients with dysgammaglobulinemia, Sjogren's syndrome, and various collagen vascular disorders [4]. It is also more common in smokers [7]. The lesion can be seen in HIV patients, but is rare. Most patients that develop MALT lymphoma are former or active smokers [6].
Treatment is surgical excision for localized disease [6]. Chemotherapy or immunotherapy (rituximab) can also be used for more extensive disease [6]. Prognosis is generally good, with a 5 year survival of over 80% [6].
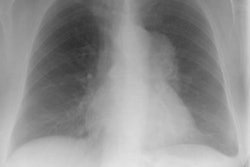
X-ray:
The lesion usually presents as a solitary pulmonary nodule (40%) and less commonly as multiple masses (20%), or as areas of alveolar consolidation. The borders of the mass are variable- ranging from sharp to hazy. Air bronchograms can be identified within the lesion. Interestingly, associated hilar/mediastinal adenopathy is uncommon, although other authors indicate that hilar and mediastinal adenopathy can be present in 30% of cases [6]. Cavitation is also uncommon. The lesions do not calcify [4]. Pleural effusions are uncommon [6]. MALT lymphoma lesions are hypermetabolic on PET/CT approximately half of the time [6].REFERENCES:
(1) Curr Prob Diagn Radiol, May/June 1996
(2) AJR 1997; Radiologic manifestations of lymphoma in the thorax. 168: 93-98 (No abstract available)
(2) AJR 1996; Lazar EB, et al. Lymphoma of bronchus-associated lymphoid tissue. 167: 116 (No abstract available)
(3) ACR Syllabus #40: p.403-404
(4) AJR 1999; Knisely BL, et al. Pulmonary mucosa-associated lymhoid tissue lymphoma: CT and pathologic findings. 172: 1321-1326
(5) Radiographics 2002; Gimenez A, et al. Unusual primary lung
tumors: a radiologic-pathologic overview. 22: 601-619
(6) Radiographics 2016; Sirajuddin A, et al. Primary pulmonary
lymphoid lesions: radiologic and pathologic findings. 36: 53-70
(7) Radiographics 2017; Bligh MP, et al. Spectrum of CT findings in thoracic extranodal non-hodgkin lymphoma. 37: 439-461