Intrathoracic Lymphoproliferative Disorders
(I would like to extend a special thanks to Dr. Darlene Metter, M.D. UTHSCSA, San Antonio, for contributions to this section)
General:
Intrathoracic lymphoproliferative disorders (LPDs) span a spectrum of benign lesions to those that are frankly malignant or have a malignant potential. The clonality of lymphoid populations is helpful in separating benign from malignant disorders. Polyclonality is usually reflective of benign disease, while monoclonality is usually indicative of malignancy. Stimulation of bronchus-associated lymphoid tissue (or BALT) and the Ebstein-Barr virus (EBV) are thought to play key roles in these disease processes. It has been postulated that the EBV genome may act as a stimulant, either as a primary or reactivated agent, particularly in disorders such as infectious mononucleosis and the post-transplant lymphoproliferative disorder.
Another important observation is that the incidence of lymphoma, both Hodgkin's and non-Hodgkin's disease, have been rising. This has been partially attributed to the Acquired Immunodeficiency Syndrome (AIDS), and an actual increase in nodular sclerosing Hodgkin's disease.
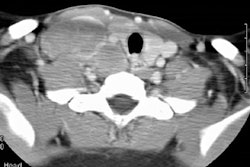
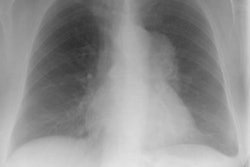
Several generalizations have been made regarding the LPDs. These are: 1- older symptomatic patients have a more aggressive disease (i.e., lymphoma); 2- benign LPDs tend to be focal (i.e., lung or lymph nodes) and pleural effusions are rare in benign disease; and 3- the post-transplant LPDs may have a variety of radiographic findings (i.e., infiltrates, masses, and/or adenopathy). The site of disease may also provide a clue to the diagnosis. Parenchymal lung abnormalities are found in association with plasma cell granuloma (pulmonary pseudotumor), pseudolyphoma, and lymphatoid granulomatosis (angiocentric immunoproliferative lesion). While mediastinal disease suggests Castleman's disease, infectious mononucleosis, or angioimmunoblastic lymphadenopathy.
REFERENCES:
(1) Curr Probl Diagn Radiol 1996; 25(3): May/June