The past few years have seen a blossoming of awareness regarding CT dose, especially in the U.S., where the detection capabilities of the latest scanners had long been considered more important than exposure levels.
And while imaging vendors, radiologists, and governments have all helped engineer dose reductions across the board, much remains to be done. There is a need for more and better mortality data -- especially the kind that do not rely on atomic-bomb survivors or great leaps of imagination. Data on the cumulative radiation dose patients receive in diagnosis and follow-up are also lacking.
The cumulative radiation burden is becoming more important now that many radiologists and would-be patients are gearing up for CT screening. The exams are leading to more findings and more follow-up than ever before, yet there are no mechanisms in place to monitor the amount of radiation patients receive throughout the course of care.
The lack of data on repeat scans led one group of radiologists to add up the numbers retrospectively for a common application -- chest CT -- based on the radiology literature. The task was complicated by a maze of different protocols that can change even in the course of a single study, but Dr. Philip Goodman and colleagues from Duke University Medical Center in Durham, NC, persevered to find some alarmingly high radiation dose totals.
Presenting his group's results at the 2002 RSNA meeting in Chicago, Goodman said there was growing concern that the injudicious use of imaging for unproven purposes could be harmful to patients.
Radiation exposure and false-positive results were the principal concerns cited at the FDA's Technical Electronic Product Radiation Safety Standards (TEPRSS) committee meeting in May of this year, Goodman said. There, committee members discussed the implications of CT screening doses that are hundreds of times higher than those seen in conventional procedures.
(Click here to download a PDF-format transcript of the FDA's Technical Electronic Product Radiation Safety Standards committee meeting on May 22, 2002. Click here to download Adobe Acrobat Reader, required to view the document.)
The TEPRSS proceedings cited a lack of scientific studies showing that whole-body CT screening is efficacious, Goodman said, "throwing into question the whole idea of radiating a population that is otherwise healthy with an unproven tool. So my message is: radiation exposure beware."
In Europe, the International Conference on Radiological Protection of Patients reported that 5 of every 100 patients can be expected to suffer fatal cancers per Sievert of exposure, Goodman said. The conference, held last year in Málaga, Spain, recommended the development of an international action plan to protect patients.
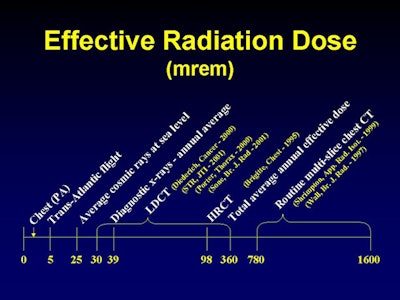
The 1.7-mrem (0.02 mSv) dose incurred with the standard PA chest film is low -- even when compared to normal U.S. background radiation levels of about 25 mrem at sea level, and to the average diagnostic imaging exam dose of 39 mrem per procedure. But while background radiation is unavoidable and a chest PA is often advisable, screening exams aren't always medically indicated, Goodman said.
His group's study used average values for the effective dose of the various CT studies to calculate the total radiation dose delivered in a year of following up a nongrowing, noncalcified lung nodule. The results showed that total effective dose was high, and that it varied significantly from study to study.
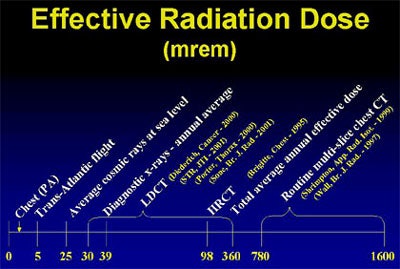 |
| Click on the image to view a larger version. Above, the radiation dose seen in various lung screening and follow-up protocols varies widely in the radiology literature. Chart courtesy of Dr. Philip Goodman. |
"In the literature, low-dose CT effective doses ranged anywhere from 30 mrem up to 360 mrem (0.5 - 3.6 mSv)," Goodman said. (The upper limit was seen in Sone et al, British Journal of Radiology, January 2001, Vol. 74:877, pp. 32-41.)
The dose from routine multislice CT chest scans ranged from 780 to 1,600 mrem, or 6-16 mSv (Wall and Hart, British Journal of Radiology, May 1997, Vol. 70, pp. 437-439; and Shrimpton et al, Applied Radiation and Isotopes, January 1999, Vol. 50:1, pp. 261-269).
These numbers coincide with the group's own experience, Goodman said, in which diagnostic multislice chest CT dose weighed in at 1,300 mrem. And techniques used in published studies often yielded far higher doses. A single high-resolution MDCT exposed the patient to 6-16 mSv, adjusted for the size of the nodule being examined, Goodman and colleagues found.
Using some protocols, screened patients are receiving 1 low-dose CT, 4-5 diagnostic CTs, 4-5 high-resolution CTs, and 5-6 scout views per year, for a cumulative effective dose of up to 40 mSv per year, Goodman said. According to the 1990 recommendations of the International Commission on Radiological Protection, such doses could create a significant risk of developing fatal and non-fatal cancers.
The original ELCAP (Early Lung Cancer Action Project) protocol, for example, recommended low-dose CT as a screening tool. If a nodule was discovered, it was followed up by a standard-dose CT and a high-resolution CT scan in the region of the nodule. Then a similar exam was performed at 30 days, after a two-week course of antibiotics, followed by yet another CT exam at 3 months, at 6 months, and perhaps another screening exam at one year, Goodman said. The radiation totals do not include scout views, each of which contributes 100 mrem (Cancer, July 1, 2001, Vol. 92:1, pp. 153-159).
"We're talking about the equivalent of 2,000 chest x-rays (per year) if you follow this protocol," he said. "I'm not saying necessarily that ELCAP's going to follow this protocol; it's a work-in-progress and things have changed. But if the initial screen finds an abnormality and then you send your patient out to some other physician for follow-up, how do we keep a handle on what's happening? How do we know they're not getting a standard CT followed by a high-resolution CT? How do we know they're not getting the equivalent of 6 chest x-rays a day every day of the year?"
When the group examined the published ELCAP data using an anthropomorphic phantom equipped with metal oxide sulfide detectors, they found a dose of 70 mrem for a low-dose chest CT, 450 mrem for a standard chest CT, and 3,800 mrem for a high-resolution CT.
"We cut the (annual) dose in half, down to 22 mSv -- that's still a thousand chest films," Goodman said. "We could calculate the number of fatal malignancies it's likely to induce using other information."
What's more, no one knows if screening works, what the optimal protocol might be, or even if screening smokers is the best approach, Goodman said. Citing a Japanese article on the efficacy and limitations of lung cancer screening, he said a recent study found 70 women with lung cancer, all of whom were nonsmokers. And 72% of the men with lung cancer had never smoked, Goodman said (Gan To Kagaku Ryoho, November 2002, Vol. 29:11:1894-1899).
"So do we even know who to screen and how often? Some are doing (follow-up) at one month, 3 months, 6 months," he said. "Some aren't screening at all, if the nodules are of a certain size, until the following year. We don't know the answer to that, but we do know that it will cost lots of money and (cause) lots of (radiation) exposure."
By Eric BarnesAuntMinnie.com staff writer
December 23, 2002
Sputum cytology gives a big boost to CT lung screening, December 2, 2002
GE, Deus to partner in lung CAD, November 26, 2002
Why CT lung cancer screening will (and won't) work, November 11, 2002
High false-positive rate seen with CT scans for lung, October 22, 2002
Whole-body CT: Radiology to the people?, October 2, 2002
Following up incidental findings may do more harm than good, September 5, 2002
Copyright © 2002 AuntMinnie.com




















