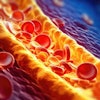
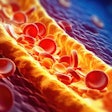
For more than 20 years, coronary artery calcium (CAC) has maintained a rock-solid association with increased cardiovascular risk and mortality. But further details are elusive.
Physicians still aren't sure how to interpret low-end calcium scores, for example, and what to tell patients when their scores change at follow-up is anyone's guess.
For despite its prognostic abilities, calcium assessment is dogged by persistent shortcomings related to accuracy and reproducibility -- problems that have intensified the search for better techniques. Some groups are working to optimize image acquisition, while others are focusing on software, or exploring alternatives to the traditional Agatston calcium-scoring method.
Radiologists discussed their efforts to improve calcium assessment at the 2002 RSNA meeting in Chicago. There, a group from Dusseldorf, Germany, concluded that two calcium-scoring software packages yielded similar results, especially among higher-risk patients. Researchers from Boston reported that mineral mass measured calcium more accurately than either volume or Agatston scores. Similarly, a Cleveland Clinic study found more interscan variability with Agatston compared to volume and absolute calcium scores.
And while their methods differ in important ways, these investigators share a common approach: that imaging techniques must be improved before calcium assessment can live up to its potential of identifying those at risk of adverse cardiovascular events.
"The coronary calcium score can help guide the initiation of clinical prevention programs as part of a risk-stratification and management scheme aimed at improving the outcomes of patients determined to be at highest risk," said Dr. Ludger Poll from Heinrich Heine University in Düsseldorf.
However, he added, it is unknown whether risk can be assessed comparably on different software packages. Poll and colleagues used identical CT data in 70 patients to assess calcium burden using two software packages: AccuImage Version 1.49 (AccuImage Diagnostics, South San Francisco, CA) and on Somatom Volume Calcium Score software (Siemens Medical Solutions, Erlangen, Germany).
All 70 patients (53 male, 17 female, mean age 48) were asymptomatic, but had known or suspected coronary artery disease. They underwent spiral CT imaging on a 4-slice Siemens Somatom Volume Zoom scanner. The standard CAC protocol included retrospective ECG gating, 4 x 2.5-mm collimation and 100 mAs. Reconstruction in the end-diastolic phase was performed using both 3-mm (incremental) slices and 1.5-mm (overlapping) slices, Poll said.
Two observers working independently performed calcium scoring using both systems. The results were divided into four categories: 0, 1-10, 11-100, and 101-400, and inter- and intraobserver reliability was calculated.
According to the results, intraobserver and intraobserver reliability were "excellent for both observers and both software systems, for each of the algorithms ranging in kappa values from 0.94 to 1.0," Poll said.
When scoring was completed on the other software package, kappa values were 0.75 for both incremental and non-incremental volume score, resulting in different risk stratifications in up to 14% of the patients. The mean Agatston score was 295 for "Software A" and 311 for "Software B," including the standard deviation.
Using the Agatston scoring method, no patients in risk groups 4 and 5 changed levels. When a single observer used identical CT data on two different software systems, risk stratification changed in 30% of patients in groups 1 to 3 with Agatston. Changing software resulted in four patients moving from risk group 1 to 2, three moving from 1 to 3, one patient from 2 to 3 and one patient downstaged from 3 to 2, Poll said.
Turning to volume scores, changing software changed the risk stratification in 17% of patients, Poll said. Four patients were upgraded from risk level 1 to 3, three patients from 2 to 3, and one downstaged from 3 to 2.
"In conclusion, interobserver and intraobserver agreement were the same in both software systems," Poll said. However, "the 2 different software systems do not yield the same calcium quantities. There were differences with regard to software reliability resulting in differential risk stratifications in 17%-30% of patients, especially in (risk) groups 1-3."
For providers, the results mean that calcium score reports should include the type of software used, Poll said, and follow-up exams should be conducted on the same hardware and software.
Are scans reproducible?
"The purpose of this study is to evaluate the variability in the quantification of predominantly mild coronary calcifications with sequential multislice CT using Agatston, volume, and mass algorithms," said Dr. Sandy Halliburton from the Cleveland Clinic in Ohio during her presentation.
The feat was accomplished in 56 patients on a 4-slice Siemens Volume Zoom scanner using ECG-triggered sequential modes with 4 x 2.5-mm collimation and 250-ms temporal resolution, she said. Then, after leaving the imaging table for a few minutes, the patients returned for a second acquisition using identical imaging parameters.
Five additional patients followed the same drill on a 16-slice scanner (Siemens Sensation 16) using improved temporal resolution (12 x 1.5 mm, 210 ms), again using sequential imaging.
Two cardiac imagers working independently calculated Agatston score, volume score, and absolute calcium mass in each of the patients for both exams.
"Interreader, intrareader, and interscan variability were calculated, and in each case the variability was defined as the absolute difference between scores divided by the average of the scores," Halliburton said. "The results were presented based on grouping from the Agatston scores: Absent plaque (0) minimal (1, 1-9); mild (2, 10-99); moderate (100-399); or severe (400 or greater)," she said.
According to the results of both readers, 66% of 224 coronary arteries imaged had no calcium on either scan. Twenty-seven arteries had no calcium on one study and an Agatston score of < 16 in the other study, according to at least one reader. Six (22%) of the remaining 50 vessels had minimal calcium, 31 mild, 13 moderate, and none severe.
Except for the very lowest calcium scores, interreader and intrareader variability remained under 5%. "However, interscan variability was a major source of problems with this technique," Halliburton said.
Flawed or not, mean interscan variability did improve as calcium burden increased for all measurement algorithms. For Agatston scoring it was 60%, 52%, and 39% for mild, moderate, and severe plaques, respectively. Volume scoring did a bit better, at 56%, 41%, and 33%, respectively. Calcium mass was the most reliable, producing 37% interscan variability for the three risk levels.
In the five patients who were examined on the 16-slice scanner, 18 of 20 arteries showed no calcium at all, leading the group to speculate that these patients' lower calcium burden may result from a lower incidence of false positives on the new machine.
"These results lead us to conclude that sequential CT is not a reproducible technique in patients with predominantly mild plaques who were included in this study," Halliburton said. "We do have confidence based on our experience that spiral (rather than sequential) CT may lead us to reproducibility, and the results of this study made us think that the increased dose necessary for (spiral CT) may be warranted."
During the question-and-answer period, however, the next speaker suggested that the likeliest cause of interscan variability is artifacts, such as motion partial-volume effect and noise, rather than the choice of sequential scanning mode.
Mineral mass beats Agatston scoring
Dr. Udo Hoffmann from Massachusetts General Hospital in Boston presented the next study, comparing the accuracy and reproducibility of traditional scoring methods, such as Agatston and volume score, with newer methods such as calibrated mineral mass and mass-equivalent ("modified Agatston") scoring.
Seeking to create the best possible imaging environment, the group performed its tests on 16 ex-vivo carotid endarterectomy specimens (carotid rather than coronary arteries because the former were available, Hoffman said). The team validated its results by means of standardized bone mineral ash phantoms used as a gold standard.
"Recently, new scoring methods such as calibration of the CT attenuation have been introduced," Hoffmann said. "This study was to compare the accuracy and reproducibility of traditional and new measurements of vascular calcification."
The researchers performed multiple segmented scans in the 16 specimens and the bone phantoms in sequential scanning mode, using a four-slice LightSpeed scanner (GE Medical Systems, Waukesha, WI). Step variations in imaging parameters yielded slice thicknesses of 0.6 mm to 5 mm, tube voltage of 80 to 140 kVp, and 10 to 150 mAs, with 500-msec rotation. Each calcium measurement method was performed for every MDCT parameter using a 90 heat-unit threshold for the presence of calcium.
"We calculated the Agatston score, and we introduced a new measurement which we call the modified Agatston score -- which uses instead of the (p)=density and density weighting factor the actual mean Hounsfield CT attenuation of the plaque," he said. "We also calculated mineral mass ... based on the assumption that there is a linear relation between pixel signal intensity and the related tissue density...We (calculated) the mineral mass volume of the ashing remnants vs. calcified volume as detected by MDCT."
According to the results, the mineral mass calculated from MDCT showed excellent precision (2.58%) and low bias (>0.0005) compared to ashing (128 ± 173 mg vs. 128 ± 173 mg).
"You see a very nice correlation," he said. "The measurements were very comparable on the mass side between multidetector-row CT and ashing, but the calcified volume as measured by MDCT (39.48 ± 55.76 mm3) was much higher than the actual volume of the ashes (339.94 ± 395.4 mm3)...MDCT using the standard protocol overestimated the calcified (volume) by about 8 times."
Calcium volume is less reproducible due to the significant influence of partial-volume effects, he said.
In addition, both the calibrated mineral mass -- and the mass equivalent or "modified Agatston" scores -- were highly reproducible amid changing imaging parameters such as slice thickness, mAs or kVp (coefficents of 5.0% and 4.9%, respectively). But traditional calcium measurements showed far more variability: The coefficient of variation was 14.5% for the Agatston method and 16% for volume scoring, he said.
"MDCT-derived mineral mass is a more accurate measurement of calcium in ex-vivo non-moving endarterectomy specimens when compared to the traditional volume score, and mineral mass and modified Agatston score are more reproducible than the traditional Agatston score," Hoffman said.
By Eric BarnesAuntMinnie.com staff writer
March 5, 2003
Related Reading
Study finds blacks have less coronary calcium than whites, February 17, 2003
Thin-collimation MDCT identifies more coronary calcium, December 18, 2002
Population-based study links coronary calcium and mortality, December 1, 2002
Technology keeps CT vital for coronary assessment, November 13, 2002
CT calcium scoring works, but what does it mean?, January 8, 2002
Copyright © 2003 AuntMinnie.com