Radiologists in the Netherlands have found that using 1.5-mm slices in electron-beam CT (EBCT) calcium scans provides results that are closer to absolute calcium mass compared with 3-mm slices, especially at lower calcium volumes.
Meanwhile, a German team examined scanners from different manufacturers, and found that quality assurance techniques are crucial for achieving consistent calcium scoring results. The two studies, presented at the 2003 European Congress of Radiology in Vienna last month, yield important clues on how scanning techniques can be used to improve the accuracy of coronary calcium screening.
Both studies measured calcium scores against standardized calcium volumes, relying on a sophisticated acrylic torso phantom developed at the Institute of Medical Physics, University of Nurnberg-Erlangen, in Germany. The phantom is built of materials that are "tissue-equivalent" for radiographic purposes. It includes lungs, testing chambers, and, for this study, cylinders of different sizes and densities filled with calcium hydroxitartrate.
For all their demonstrated prognostic value, the reproducibility and accuracy of EBCT calcium measurements have been questioned, said Dr. Rozemarijn Vliegenthart from Groningen University and University Medical Center in Amsterdam. "Scanning with thinner slices than the current standard may improve accuracy," she said.
Her group sought to compare the accuracy of non-overlapping 3-mm and 1.5-mm (60 slices) techniques in the quantification of absolute calcium mass, both in the phantom and in a study population. Exposures were the same for both the plastic and the people: 1.5-mm and 3-mm slices were acquired using an Imatron C-150 electron-beam scanner (GE Medical Systems, Waukesha, WI). Scan time was 180 seconds, FOV was 260 mm. Modified calcium volume scores were calculated using isotropic interpolation with software from AccuImage Diagnostics of South San Francisco, CA. The threshold for the presence of calcium was 130 HU across a minimum of 2 adjacent pixels.
"The calcium cylinders had three different densities and three different diameters," Vliegenthart said. "Diameters were 1, 3, and 5 mm, and densities were 200, 400, and 800 mg per cubic cm of calcium hydroxitartrate."
In the 1,302 subjects (mean age 71 years, M/F:48%/52%) the two single-breathhold scans were performed within minutes of each other; patients were not moved in between scans. ECG triggering was performed at 80% RR interval. The effective radiation exposure was 0.8 mSv for the 3-mm scan, and 1.5 mSv for the 1.5-mm scan.
Only results from the 3-mm and 5-mm cylinders were reported due to the poor visibility of the 1-mm cylinders. But the phantom results, expressed in terms of the deviation of calculated volumes from the true cylinder volumes and in the variation in measurements, was higher overall for the 3-mm scans.
"For 1.5-mm scans, the variation coefficients ranged from 1.8% to 9.5%, but for 3-mm scans they ranged from 3.2% to 10.3%," Vliegenthart said. "In two-thirds of the cases, the variation was smaller for 1.5-mm scans than for 3-mm scans. The 3-mm cylinder had a volume of 21 cubic ml. When we looked at the volume scores, we see first of all that with increasing calcium density, the volume scores go up for both the 1.5- and 3-mm scans."
The result is an overestimation of calcium volume in both 1.5- and 3-mm scans, as high as three times actual density. However, the results of the 1.5-mm scans were much closer to the actual calcium densities in the cylinders.
Among the living subjects, the median calcium volume score was 100 (interquartile range: 11-409) for the 3-mm protocol, and 144 (interquartile range: 35-513) for the 1.5-mm protocol.
"Twenty-eight percent of the subjects were classified in a different (risk) category (between) the 1.5- and 3-mm scores," she said. "And in fact 90% of those categorized in a different category went to a lower category for the 3-mm scan," differences which could affect the stratification and future treatment of these patients, Vliegenthart said.
"EBCT scans with a slice thickness of 3 mm (yielded) less accurate calcified volume than 1.5-mm slices," probably due to reduced partial-volume effects, she concluded. "The use of thinner-slice protocols considerably affects the classification of individuals based on the amount of coronary calcification."
Future studies should focus on the question of whether thinner slices improve the detection of coronary calcification, risk stratification, and outcomes in clinical practice, she added.
In response to audience questions, the results do not yet constitute sufficient grounds to obtain thinner slices in all CAC screening patients, she said. However, the group is methodically following up patients in an effort to obtain long-term outcome data that might demonstrate any clinical benefits associated with the thinner-slice protocol. If outcomes can be improved, the increased radiation exposure associated with thin-slice protocols will be justified, Vliegenthart said.
An audience member predicted that thinner slices will prove more accurate in patients with less calcium, but added that "when you reach a score of 300-400, then you just double the (radiation dose) using 1.5-mm slices."
QA yields cross-scanner consistency, minimum dose
In another presentation, researchers from the Institute of Medical Physics at the University of Erlangen, Germany, used the same torso phantom to standardize calcium scoring results across "different scanners and different scanning techniques," Stefan Ulzheimer, Ph.D., said in his presentation.
Ulzheimer, along with Kaiss Shanneik and CT pioneer Willi Kalender, Ph.D., assessed spatial resolution on the x, y, and z axes, and also evaluated contrast and noise. They scanned coronary calcium inserts in the phantom with small calcifications from 1-5 mm and calcifications using cylinders with a variety of densities of calcium hydroxitartrate on the different scanners.
The scanners included a LightSpeed 16 and Imatron Evolution C-150XP (GE Medical Systems Waukesha, WI), an Mx8000 Quad/IDT (Philips Medical Systems, Andover, MA), a Sensation 4/16 (Siemens Medical Systems, Erlangen, Germany), and an Aquilion Multi/Multi 16 (Toshiba America Medical Systems, Tustin, CA).
"We always use the scan protocols recommended by the manufacturers for the quantification of coronary calcium," Ulzheimer said, noting that Siemens is the only manufacturer that recommends the spiral protocol for the assessment of coronary calcium.
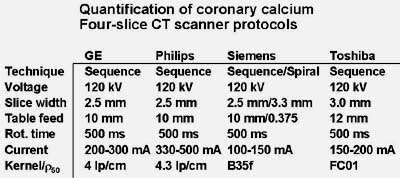 |
| Above, manufacturers' recommended coronary calcium assessment protocols. Chart courtesy of Stefan Ulzheimer, Ph.D. |
"There is good agreement between the scanners if you calculate the Agatston scores," Ulzheimer said. "The larger the calcifications and the more dense the calcifications are, the better the agreement.... The largest deviations (in Agatston scores) are of course up to 60%, 70%, 80% depending on the protocol used. The same applies if you calculate the calcium mass, and the deviation among the scanners (increases) as the calcium masses get more robust." However, inter-scanner reproducibility was significantly worse using Agatston scores (5-56%) compared with calcium mass (6-16%).
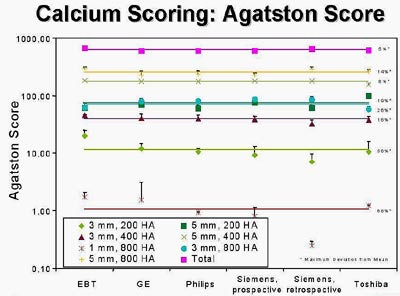 |
| Agatston scores are consistent across scanner models for lower calcium levels, but less consistent as calcium density increases. Chart courtesy of Stefan Ulzheimer, Ph.D. |
The group also assessed image noise for small, medium, and large patients on the different scanners. Image noise increases, of course, for larger patients, he said. The noise data can be used to adjust the mAs downward for each scanner and patient size to arrive at a consistent noise level of 20 HU, for example.
"This leads to a defined image quality with respect to noise, and you even get a dose reduction...of 10% to 80% from the different protocols," he said.
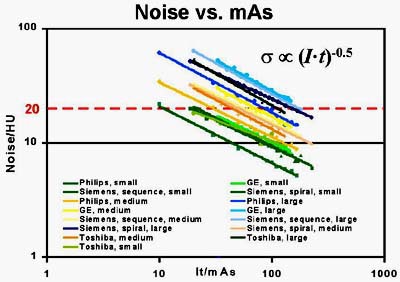 |
| Image-noise levels vs. mAs for different scanners and patient-size protocols. Noise levels varied considerably, between 9-24 HU. Chart courtesy of Stefan Ulzheimer, Ph.D. |
Quality assurance is essential for achieving comparable cardiac image quality in different CT scanners, Ulzheimer concluded. "The QA tools presented here are able to assess all important image quality parameters. And those parameters have to be defined for standard applications such as CTA or coronary calcium scoring to guarantee high-quality quantitative measurements," he said.
The group will also use its tools and testing methods to evaluate new scanner models and new scanning techniques, Ulzheimer said.
By Eric BarnesAuntMinnie.com staff writer
April 16, 2003
Related Reading
Standard, low-dose CT calcium screening yield equivalent results, March 10, 2003
New techniques boost accuracy of coronary calcium assessment, March 5, 2003
Study finds blacks have less coronary calcium than whites, February 17, 2003
Thin-collimation MDCT identifies more coronary calcium, December 18, 2002
Population-based study links coronary calcium and mortality, December 1, 2002
Technology keeps CT vital for coronary assessment, November 13, 2002
Copyright © 2003 AuntMinnie.com