Plowing through the very investigational field of MR colonography (MRC), researchers from the Prince of Wales Hospital in Hong Kong used air as a contrast agent to look for colorectal polyps and carcinomas in 22 patients. Their MR technique is feasible, the group concluded, but has a low sensitivity for the detection of polyps smaller than 1 cm.
Dr. Nina So, Dr. Wynnie Lam, and colleagues from the departments of radiology and surgery wrote that although a number of studies have used MRI for virtual colonoscopy, most have relied on liquid contrast agents, which can be troublesome in clinical use, and tend to slow patient throughput.
"To date, most of the MR colonography studies have used water-based agents for intraluminal contrast," the authors wrote in this month's Clinical Radiology. "These include gadopentetate dimeglumine and water enema, iron glycerophosphate enema, and manganese chloride and barium water mixture. Colon insufflation using room air or carbon dioxide has been used in CT colonography without undue patient discomfort. However, there are only a few reports on the use of a gaseous medium as intraluminal MR contrast media: air, CO2 enema, and hyperpolarized helium have recently been reported" (Clinical Radiology, July 2003, Vol. 58:7, pp. 555-559).
Air is not only free and abundant, it is easy to administer, the group wrote of their choice of contrast. Air is commonly used in CT virtual colonoscopy owing to its high intrinsic contrast with the colonic wall, and was also used successfully in a recent German MR virtual colonoscopy study.
In the Hong Kong study, 22 patients scheduled for conventional colonoscopy due to a change in bowel habit and positive occult bleed underwent MR virtual colonoscopy (MR colonography or MRC) and conventional colonoscopy on the same day.
The patients first underwent standard bowel preparation with a phosphate soda prep. Before the procedure began, patients also received 1 mg of glucagon hydrochloride (Novo Nordisk, Bagsvaerd, Denmark). Then, with the patient lying in a decubitus position, a Miller balloon and 14-French feeding catheter was used to gently insufflate air to the colon, and was stopped when the patient began to feel uncomfortable.
Body-array, flex large, and spine-array coils were used to acquire MRC images on a 1.5-tesla Sonata scanner (Siemens Medical Solutions, Erlangen, Germany).
"MR colonography was performed using the single-shot half-Fourier rapid acquisition with refocused echos (RARE) technique described by Morrin et al," the authors wrote (American Journal of Roentgenology, 2001, Vol. 176:1, pp. 144-146).
The entire abdomen was imaged in four to five consecutive contiguous axial breath-hold acquisitions, each with 24 contiguous slices (TR 1,000 ms, effective TE 65 ms, matrix 256 x 134, 4-mm slice thickness, flip angle 150°, TA 24s, and field of view from 300 to 400 mm. The sequence was repeated with two coronal acquisitions using the same parameters, according to the authors.
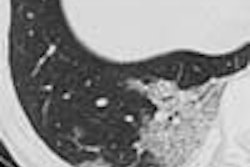
Two radiologists, blinded to the conventional colonoscopy results, evaluated the images and reached their diagnoses by consensus, dividing the colon into five segments and also grading the distension quality from 1 (poor) to 3 (adequate). Lesions were diagnosed when suspected polyps failed to move between prone and supine imaging sequences, and the results were compared with those of conventional colonoscopy.
According to the results, 105 (95.5%) of the 110 colonic segments were evaluable (score of 3), with only 5 (4.5%) receiving a score of two and no segments scoring 1. Image quality was good in all cases. Two patients with poor bowel prep at colonoscopy were excluded from further study.
"Three lesions were found by MR colonography," the authors wrote. "These consisted of a polyp measuring 1 cm in the sigmoid colon, a 2-cm rectal carcinoma, and an 8-cm-long circumferential tumor at the transverse colon."
Conventional colonoscopy detected all of these lesions in addition to 12 polyps 5 cm and smaller, and one polyp measuring 7 mm, that were not seen on MR. Even retrospective review of the MR data did not reveal these polyps, and the authors suggested that the relatively thick 4-mm slice acquisitions might have been responsible for MR colonography's low sensitivity.
"The spatial frequency blurring associated with the RARE sequences may have also contributed to this underdetection of small lesions," they added.
"However, the image quality permitted adequate visualization of the interface between air and colonic mucosa in all cases," So and colleagues wrote. "The long train of refocusing echoes used in the single-shot half-Fourier RARE sequence potentially leads to more heat deposition within the tissues than the traditional spin-echo sequences. However, the recommended specific absorption rate (SAR) had not been exceeded in our study, and none of the patients complained of any discomfort."
A potential benefit was seen in the subsecond image acquisition of the RARE sequence, which effectively freezes movement in the diaphragm. As a result, images are less likely to be blurred than in turbo spin-echo sequences, which are more sensitive to respiratory and peristaltic movements, the authors wrote.
"In patients with incomplete colonoscopy due to stenotic tumor ... this technique was useful in demonstrating the mucosa of the more proximal colonic segments and excludes the presence of clinically significant lesions," they wrote.
Future large-scale studies with optimal bowel preparation, coils, and imaging protocols might improve MR results further, the group concluded. "But for the detection of smaller lesions, CT colonography performed with the multidetector CT is likely to be more sensitive," they said.
By Eric BarnesAuntMinnie.com staff writer
July 15, 2003
Related Reading
German group optimizes barium-sulfate tagging in MR colonography, January 22, 2003
Copyright © 2003 AuntMinnie.com