The Mayo Clinic doesn't offer whole-body CT screening, not really. Not if you mean the take-all-comers, heck-with-follow-up kind of scans sold at shopping malls like stressed denim. Not Mayo. But if you're talking about the careful CT assessment of adults who happen to be asymptomatic, well, in that case the Rochester, MN-based practice might be able to help.
Is there a difference? There is, and it's as clear as night and day to Dr. Frank Earnest, who directs CT practice for the academic multispecialty group and serves as a member of its outpatient practice committee. He emphasizes that Mayo whole-body CT isn't a whole-body exam at all, but one "performed from the top of the chest to the pelvis."
Unfortunately, Earnest said, CT screening has come to mean the scanning of self-referred, asymptomatic subjects who are quickly given the results, then either left to manage their own follow-up or find a primary physician to do it for them. Such exams are rarely correlated with other studies or with the patient's medical history, he said. They're often discounted, sold in package deals, or, according to numerous Web sites, even marketed as gifts for loved ones.
In contrast, the Mayo model brings "true multispecialty integration" and a "focus on the patient" to CT screening, Earnest explained at the 2003 International Symposium on Multidetector-Row CT in San Francisco. The practice requires a personal physician to make the referral for any exam, which is unhurried and cautiously undertaken. The patient is given ample opportunity to discuss symptoms and suspicions. The results are correlated to any previous studies, and to the patient's medical history, and there is a fee.
Mayo offers two types of screening, he said. Type 1 consists mainly of research, such as the Mayo Screening Study, the National Lung Screening Study, and the Mayo Colonography Trial, for example. The subjects are enrolled free of charge.
Then there's Type 2. "I call this the Trojan Horse screening," Earnest said. "These are patients who request an exam and have a physician who's agreeable (to it) in our practice. Typically there are vague indications listed, such as cough or abdominal pain, and... typically these kinds of indications are probably for the benefit of the insurance company or third-party payor. A lot of times there's no mention of the particular complaint in the medical record. (Screening CT) is sometimes performed on otherwise healthy subjects, although most patients have some concern that we are addressing; very few are just interested out of serendipity."
But even with all due attention paid to indications, appropriateness, and education, screening can be frustrating and time-consuming for both the patient and the radiologist. Earnest cited the case of a 52-year-old man who underwent thoracic CT screening with IV contrast. The radiologists found two benign-looking lung nodules that the patient elected to follow up while outside the U.S.
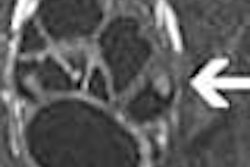
"But we found three liver lesions as well, and now what do you do? I think there are three different routes you can take," Earnest said. "One is just to call them indeterminate and ask them to get followed up along with the lung nodules. The second alternative perhaps is just to say they're benign. We know statistically in patients without cancer and even those with cancer, well-circumscribed hypodense lesions in the liver can be benign. Finally, we can go to the more-intensive investigation and get ultrasound plus or minus biopsy. Well, (the patient) was kind of a need-to-know guy, and we ultimately ended up doing ultrasound, and (found) hyperechoic lesions without halos, well circumscribed. We thought these were benign, probably cavernous hemangiomas, and that was the end of it."
Finally. But despite the frustration of the thing, Mayo researchers have succeeded in producing some of the most important statistics available in CT screening, especially those resulting from two recently published studies. The first, by Dr. Steven Swensen and colleagues, examined 1,520 smokers 50 and over with 20 or more pack years (Radiology, March 2003, Vol. 226:3, pp. 756-761).
The subjects underwent three annual low-dose CT exams of the chest and upper abdomen, with findings of 2,832 uncalcified pulmonary nodules in 1,049 participants (69%). The researchers diagnosed 40 cases of lung cancer (2.6% of patients), including 26 at baseline CT and 10 at subsequent annual exams. Twenty-one (60%) of the 35 non-small cell cancers detected at CT were stage IA at diagnosis, and the group also identified 690 additional findings of clinical importance.
"So it's important to recognize that when we look at these screening CT exams, we frequently miss small nodules the first time around," Earnest said.
Heading south from chest to abdomen, Earnest cited another recent Mayo study that examined extracolonic findings in virtual colonoscopy (CT colonography) of 681 asymptomatic subjects, as well as the short-term medical costs of follow-up (Gastroenterology, April 2003, Vol. 124:4, pp. 911-916).
Extracolonic findings were common, and found to be of high clinical importance in 71 (10%) of the individuals, of medium importance in 183 (27%), and of low importance in 341 individuals (50%). Subsequent medical or surgical interventions resulted from these findings in 9 patients (1.3%). The average added cost per VC examination was $34.33.
"Twenty-seven percent had a finding for which follow-up was recommended," he said. "This represents a significant burden to the patients. We know that at least half the patients in our practice who have a lung CT will be coming back for follow-up exams; at least 27% or maybe a third of patients who have abdominal imaging ... will need follow-up. If you drill down on that data and look at the patients who actually received treatment for those findings, there are 1 1/2% of patients that had operations on their lung, and 1.3% of patients that had other surgical interventions. So our anticipated yield with one screening chest CT is 50%; our anticipated yield of 'positive findings' that we recommended follow-up for in abdomen and pelvis scanning for colonography without IV contrast was 27%."
Fairly high, in other words. So how does this experience shape the Mayo treatment model? Understanding the incidence of abnormal findings helps inform the decision-making process, as well as the patients and physicians, Earnest said. One of the hallmarks of the Mayo model is having a personal physician who listens to patients' needs and directs care their patient care over time, working with the local physician and the referring physician.
"This differentiates and perpetuates our practice," Earnest said. "Secondly, it attracts the right people to our practice. When we recruit physicians ... it's important that they know what our healthcare principles and values are. I think it also means consistency for the brand, and I know that's a kind of crude term for healthcare, but it's part of the patient's expectations. You know, brand is consistency, and variability in that product really devalues the brand."
The group has developed a written statement of its values and care model in an effort to preserve what it considers unique and valuable about the practice, particularly in light of its growth to new sites and accompanying influx of new faculty and staff. The clinical education staff and clinical practice committee have also been working on a series of brochures for patients and for referring physicians covering different screening exams.
Radiologists play a central role in both education and decision-making, Earnest said. With their specialized knowledge of imaging procedures, they are in a unique position to educate staff and referring physicians about the benefits, risks, and alternatives for imaging.
Before screening, patients are also given a feel for where imaging might lead, he said. Finding a nodule might lead to a biopsy, which is generally safe, but could lead to a tube for pneumothorax, or in a few patients even hemoptysis, they are told.
"If we do a biopsy on a small nodule, there's a chance that it could be cancer and we might miss it," Earnest continued. "And death is reported but extremely rare, but these are the kinds of things we need to at least allude to in our patients who are undertaking screening."
"We don't feel like we're ready to do a whole lot of screening whole-body CT," he said. "We feel that probably it has yet to be shown whether this has a whole lot of benefit. And in our practice we feel it's something we should do only after we inform the patients about the incidence of positive findings that are probably not of any significance to their health."
By Eric BarnesAuntMinnie.com staff writer
October 3, 2003
Related Reading
Guidelines sought for self-referred imaging amid ethical concerns, August 14, 2003
Reimbursement gains, competition prime CAD market, July 15, 2003
Whole-body CT picks up renal cell carcinoma in asymptomatic patients, May 28, 2003
Whole-body CT: Greater than the sum of its parts?, May 20, 2003
Legal issues shadow CT screening, February 27, 2003
Copyright © 2003 AuntMinnie.com