Some virtual colonoscopy providers are working to improve the technique with multislice CT scanning and thin-section reconstructions; others are experimenting with stool tagging and computer-aided detection (CAD) of suspected lesions.
Another potential aid, intravenous contrast enhancement, has gotten a cooler reception from providers who are understandably wary of adding to the cost or risk of virtual colonoscopy. But a growing body of literature demonstrates that IV contrast is the right choice in certain patients.
At the 2003 International Symposium on Virtual Colonoscopy, Dr. Martina Morrin from Beth Israel Deaconess Medical Center in Boston discussed the situations in which contrast-enhanced CT is making a difference.
"I'm not advocating that IV contrast be performed as the standard (virtual colonoscopy) technique, but I think there is a potential impact in certain patients," Morrin said. "It can be used as a problem-solving tool in trying to detect whether a lesion is a stool or a polyp. It may be used (to enhance) the detection and characterization of certain lesions, and as a salvage approach in poorly prepared patients."
Certainly, dual positioning in the prone and supine positions has improved the ability to differentiate stool from polyp, she said, but it doesn't completely solve the quandary of interpreting findings that lack the "smooth morphology of polyp," yet do not retain air or move when the patient turns from supine to prone. In suboptimally prepared colons, which account for a significant number of VC exams, IV contrast can enhance and help identify submerged lesions. To date, fecal-tagging results have been inconsistent, and the technique remains experimental, she said.
A study at her facility has demonstrated the utility of IV contrast in suboptimally prepared colons.
"Contrast-enhanced virtual colonoscopy was performed on 81 consecutive patients, 48 of whom received intravenous contrast (150 cc of Optiray (Tyco Healthcare Mallinckrodt, Hazelwood, MO) at 3 cc/sec), with scanning initiated 45 seconds after administration of the initial bolus," Morrin said.
The patients were scanned in a single breathhold in the supine position, then the contrast was administered and prone images were acquired. The use of contrast yielded significant advantages, especially in its improvement in the detection of medium-sized polyps (6-9 mm) from 58% to 75% (p<0.05).
"In addition, three large polyps in our study were detected only with the use of intravenous contrast, one of which was a high-grade dysplasia," she said. "Using a five-point scale, overall reader confidence improved significantly (with the use of contrast), as (did) bowel wall conspicuity," Morrin said. "We found that only 19% of patients had a completely clean colon at the time of the study.... Fifty-nine percent of patients had some residual fluid, and 13% of patients had adherent stool, or fluid that did not displace when the patient was moved from supine to prone position (Radiology, March 2000, Vol. 217:3, pp. 765-771)."
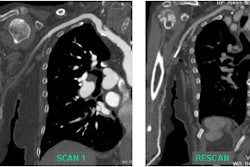
"This is an example of a supine non-contrast scan: 50% of the lumen is occupied by residual fluid...When you administer intravenous contrast you can see that this wall is very nicely seen on the prone scan and the contrast," said Morrin, who also noted that contrast improves the ability to detect the flat or sessile lesions frequently missed on virtual colonoscopy exams. Residual fluid in the sigmoid and ascending colon is particularly resistant to elimination when the patient changes position, Morrin wrote in an accompanying abstract.
In a study published last summer, the group sought to determine whether the use of IV contrast in VC could help predict malignant differentiation of colorectal neoplasms 10 mm and larger. Patients underwent virtual colonoscopy on four-detector scanners using 3-mm collimation, pitch 2, 120 mAs and 120 kVp, using the same contrast protocol as for the 2000 study above. Images were reconstructed at 1.5-mm intervals with a 1.5-mm section overlap. Enhancement of 29 consecutive neoplasms, all histologically proven, was measured retrospectively, both before and after the administration of IV contrast.
"There was no correlation between the size and the enhancement of the lesion...(but) we did find a correlation between cancer grade and perfusion," Morrin said.
There was a trend toward increasing enhancement from adenoma with dysplasia (grade 2) into poorly differentiated adenocarcinoma (grade 5), though it did not reach statistical significance, the group wrote. They found tumor perfusion to be varied and unpredictable, and suggested that using a variety of contrast protocols, and perhaps contrast agents targeted specifically to detect angiogenesis, might have improved the results (Radiology, July 2003, Vol. 228:1 pp. 152-156).
In an earlier IV contrast study, Morrin and colleagues found the technique useful for preoperative planning in patients suspected of having extensive colorectal cancer, by identifying the invasion of pericolic fat planes, adjacent organs, and metastases, especially of the liver (Diseases of the Colon and Rectum, March 2000, Vol 43:3, pp. 303-311).
In that study, "(VC) correctly staged 13/16 colorectal cancers," she said, adding that all 13 correctly staged patients had received IV contrast, while all three incorrectly staged cases did not receive contrast.
The extracolonic findings might even reduce the need for separate contrast-enhanced CT follow-up scans in cases of low clinical importance, and thus avoid some duplication of effort, she said, citing the findings of Gluecker et al (Gastroenterology, April 2003, Vol. 124:4, pp. 911-916).
Other research suggests that as many as 10% of extracolonic findings may be of high clinical importance. And a new study by Dr. Roberto Iannaccone and colleagues in Rome confirmed the utility of contrast-enhanced CT for colorectal cancer staging. Another study by the same group (in this case led by Dr. Andreas Laghi) recently reported that contrast-enhanced VC may be a feasible alternative to surveillance (conventional) colonoscopy, liver ultrasound, and chest x-ray in patients who have undergone resection for colorectal cancer. Among the 35 patients, colonic evaluation was judged as optimal in 91.7% of all colonic segments (European Radiology, June 2003, Vol. 13:4, pp. 883-889).
Also in 2003, researchers from Turkey sought to determine whether the use of IV contrast could help distinguish benign colorectal lesions from residual fluid, Morrin said. In a small survey, the group found that benign polyps and carcinomas enhance significantly following contrast administration. The use of IV contrast in VC may help differentiate solid lesions from residual colonic fluid that does not enhance, they concluded (European Radiology, July 2003, Vol. 13:7, pp. 1,657-1,663).
In terms of limitations, the use of contrast adds $60-$70 to the cost of the exam, and can lead to reactions in a small number of patients. Even with contrast, virtual colonoscopy does a poor job of detecting polyps 5 mm and smaller. "One problem is large lesions; it can be difficult to determine if these are stool," she said.
The Beth Israel researchers currently administer IV contrast to patients whose prep is deemed suboptimal in initial supine scanning, and specifically in patients with pools of residual fluid greater than 2 mm in depth. The facility also uses the technique in patients with colorectal masses -- for the evaluation and characterization of wall invasion, lymphadenopathy, and liver metastases.
"It definitely has a role as a salvage approach in patients with poorly prepared colons," she said. "It definitely has a role in problem-solving ... and it may have a role in the staging of tumors." Larger, randomized trials will be needed to validate the benefits of contrast enhancement in virtual colonoscopy, she concluded.
By Eric BarnesAuntMinnie.com staff writer
January 19, 2004
Related Reading
Results suggest important new cancer staging role for virtual colonoscopy, December 19, 2003
Virtual colonoscopy techniques evolve with technology, July 25, 2003
Virtual colonoscopy: to contrast, or not to contrast, April 10, 2002
Copyright © 2004 AuntMinnie.com