VIENNA - Multislice CT found more diminutive colorectal polyps than MRI in an acrylic phantom, but high-field MR scanners may be capable of closing the gap. In a study presented today at the European Congress of Radiology, Dr. Roman Fischbach from the University of Muenster in Germany compared virtual colonoscopy in both modalities using four scanners: CT in 4- and 16-slice models and MRI in 1.5- and 3.0-tesla machines.
"CT as well as MR colonography has been shown to be acceptable in patient studies, but CT has been much better accepted with the introduction of multislice CT scanners, and I think that in the next years we will see a competition between the two modalities for patients and applications," according to Fischbach.
"CT is widely available, it’s inexpensive compared to MR, it’s quick, simple, and has high spatial resolution, but the drawbacks are, depending on the scan protocols involved, potentially nephrotoxic contrast injections and certainly also the radiation exposure," he said (Iodinated contrast is not used in the majority of CT virtual colonoscopy studies).
In the study, Dr. Johannes Wessling, Fischbach, and colleagues decided to pit the modalities against each other. They built a Dubliplast dental plastic phantom with simulated haustral folds and 10 mostly small polyps (including 3 x 2 mm, 3 x 3 mm, 3 x 4 mm, 1 x 6 mm, and 1 x 8 mm lesions). The ersatz colon was placed in a water-filled cylinder to simulate the absorption of the average body, and then packed in margarine to simulate tissues, surrounded by another layer of acrylic.
CT images were acquired using 4- and 16-slice CT scanners (Volume Zoom and Sensation 16, Siemens Medical Solutions, Erlangen, Germany) using the highest spatial resolution possible: 4 x 1-mm and 16 x 0.75-mm slice thicknesses and reconstruction increments of 1.25/0.6 mm and 0.75/0.5, respectively, pitch 1.2, with 100 mAs and 120 kVp for both scanners.
MRI images were acquired using 1.5-tesla and 3.0-tesla Gyroscan scanners (Philips Medical Systems, Best, the Netherlands) using an ultrafast 3-D GRE VIBE sequence, fov 350 mm, flip angle 5°, matrix 10 x 256, and a slice thickness 1.4 mm for each field strength.
"The image assessment involved almost the entire department," he said. "We had 20 radiologists to evaluate the location of polyps, split up in groups of five; four for every modality, and we only looked at volume-rendered images, and we only wanted to identify the polyps and grade the image quality (subjectively) on a scale of two to four." Comparisons of sensitivity were performed using the Wilcoxon test for paired data.
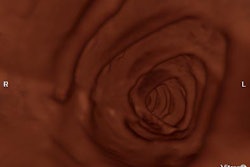
"Using the 16-slice CT scanner represents quite easily visible polyps...you can see that using the MR approach the bigger polyps are seen in a fashion quite similar to the CT depiction, however the small lesions...are almost not visible."
Pooled data from all readers showed a slight advantage for the 16-slice high-resolution scanner versus the four-slice CT machine, and for the 3.0-tesla scanner compared to the 1.5-tesla machine, (p=0.83 and p-0.12, respectively). However, neither of these differences was statistically significant.
The conspicuity of the polyps detected was similar among the modalities and models, though there was a slight trend toward better delineation in CT, but again, it was not statistically significant, Fischbach said.
However, owing to superior spatial resolution in the four-slice CT scanner compared to the 1.5-tesla MR scanner, sensitivity was much higher for the smallest polyps on CT. The results showed that the overall sensitivity for polyp detection was 93% for the 16-slice CT scanner, 87% for the 4-slice scanner, 51% for the 1.5-tesla scanner, and 50% for the 3.0-tesla scanner.
All four machines picked up 100% of polyps larger than 6 mm, while the sensitivity for the detection of polyps 4 mm and smaller was significantly higher for CT (4-slice: 88%; 16-slice: 83%) compared to MRI results (1.5-tesla, 39%; 3.0-tesla, 38%, p=0.001).
"You can summarize that for polyps bigger than 6 mm, there’s no problem for either modality," Fischbach said. "Smaller polyps can only be reliably detected by CT using the spatial resolution given by the MR protocol. We have about 25% better spatial resolution, but it had no significant impact on the detection of the 2-3-mm lesions. So we can conclude that CT is required if you want to detect the smaller, probably clinically irrelevant polyps -- but the relevant lesions are seen in both modalities."
But there’s more to the story. First, it is logical that the 16-slice CT scanner would not pick up any more lesions, as its maximum spatial resolution was already sufficient in the 4-detector machine. "The smallest polyp was 2 mm, and we used a 1-mm slice thickness or a 0.75-mm slice thickness (4- and 16-slice CT scanners, respectively), so this is thin enough to detect every lesion that is 2-mm or larger," Fischbach said.
Moreover, the 3.0-tesla MR scanner could have achieved higher spatial resolution than it did. The maximum spatial resolution for the 1.5-tesla MR scanner was 1.4 mm, "so if you don’t get the slice right on the polyp you can miss it," Fischbach told AuntMinnie.com.
And because the 3.0-tesla machine produces three to four times the signal of the 1-5-tesla machine, it is consequently capable of higher resolution, potentially enough to see even the smallest polyps. But the 3.0-tesla scanner was installed midway through the study, and so its resolution was not maximized, but rather matched to the level of the 1.5-tesla machine (at 1.4 mm) for the sake of continuity.
Thus, if the spatial resolution of the 3-tesla MR were maximized, "we could either reduce the scan time or decrease slice thickness or increase the matrix," Fischbach said. "So the 3.0-tesla scanner should produce better results in the future once we optimize the protocol."
By Eric BarnesAuntMinnie.com staff writer
March 8, 2004
Related Reading
U.K. rads perform most VC with contrast, but on a limited basis, February 16, 2004
Experience sharpens role of IV contrast-enhanced VC, January 19, 2004
RARE technique shows benefits in MR colonography, July 15, 2003
German group optimizes barium-sulfate tagging in MR colonography, January 22, 2003
Copyright © 2004 AuntMinnie.com