It's said that the best colon screening exam is whichever one people are willing to have, but most still choose none of the above. Less than half of the U.S. population over 50 has had a colonoscopy or sigmoidoscopy, for example, and the relatively uncomfortable bowel prep is often cited as a key factor underlying their skittishness. To be sure, virtual colonoscopy is less invasive than the conventional exam, but it still requires purgative bowel cleansing for optimal performance.
Still, researchers are continuing their efforts to perfect stool tagging and digital subtraction techniques, hoping to someday make virtual colonoscopy easy enough for the masses -- and potentially save many lives. Radiologist Dr. Michael Zalis, who heads up CT colonography at Massachusetts General Hospital in Boston, is a leader in this pursuit. At the 2003 Symposium on Virtual colonoscopy in Boston, he discussed recent progress -- and some remaining difficulties -- in stool tagging and digital subtraction.
Zalis said that data from his institution suggest two trends that seem to be affecting the interpretation of minimal-prep exams. First, he said, the presence of tagging agents does render retained fecal material distinct. As a result, the interpreting radiologist is less likely to mistakenly interpret it as a false-positive lesion.
"The second thing is that there has been a (downward) shift in our likelihood to call smaller diminutive lesions, which traditionally have accounted for a lot of false-positives in CT colonography," he said. "I think we're far less likely to call small lesions in general."
Indeed, no false-positives were reported among the 60 minimal-prep VC patients imaged so far in a pilot study at his institution, Zalis told AuntMinnie.com, probably to the credit of both trends, he added. And while false-positives may yet appear as the cohort grows larger, the results so far "strongly suggest that minimal-prep technique contributes to increased specificity -- i.e. decreased likelihood of making a false-positive call," Zalis said.
Other investigators have also found utility in stool tagging. Drs. S. Gryspeert, Philippe Lefere, and colleagues at Stedelijk Ziekenhuis in Roeselare, Belgium, found that a reduced-cleansing regimen based on a low-residue diet, bisacodyl, magnesium citrate, and a dedicated barium suspension reduced preparation-related discomfort significantly over traditional cleansing methods, while fecal tagging with barium reduced the incidence of false-positives (JBR-BTR, December 2002, Vol. 85:6, pp. 289-296).
The same group also published an earlier study of 100 patients. Fifty patients underwent polyethelyne glycol cleansing before VC, and another 50 had a 2.1% oral barium fecal-tagging regimen. The researchers found comparable sensitivity and increased specificity using the fecal-tagging regimen (FT specificity, 88% [30 of 34 patients]; non-FT, 77% [23 of 30 patients]). Patients were slightly inclined to favor the FT regimen as well, but the trend was not statistically significant.
In his 60-patient pilot study, Zalis' group used different shades of minimal prep, along with the contrast method originally reported in a 2003 study of digital subtraction techniques (Radiology online, January 24, 2003).
Taken with meals 48 hours before CT "...the contrast material regimen consisted of 8-mL aliquots of nonionic iodinated oral contrast material (Oxilan 300 [300 mg of iodine per milliliter], Cook Imaging, Bloomington, IN)," the authors wrote in Radiology.
Following patient-controlled insufflation of the colon with room air, prone and supine CT images were acquired on a four-detector-row LightSpeed QXi scanner (GE Healthcare, Waukesha, WI). The low-dose technique included 140 kVp, 50 mAs, 0.8-second scan time, 6:1 pitch and soft-tissue reconstruction.
However, the results of fecal tagging without digital fecal subtraction have been disappointing, Zalis said. Rating image quality on a subjective five-point scale, one being uninterpretable and five being fabulous, the group recorded lower scores than it had hoped for in its 60-patient pilot study.
"Only 50% of the time using just a tagging agent with nothing else on board did we achieve what we considered a really excellent homogeneous semi-liquid labeling contrast," Zalis said in his presentation. "So I think this is pointing to an area where we're going to have to do a little bit more work on the preparation before it's ready for prime time."
Not the only problem
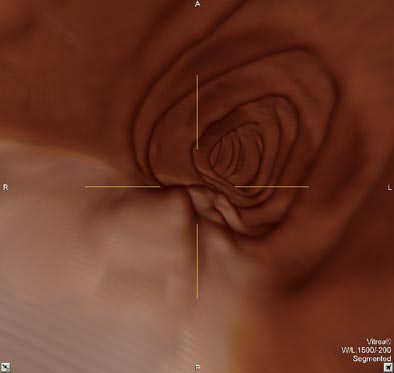
Stool tagging brings up another nettlesome issue, too: the potential of high-density stool tagging to distort lesion size in automated digital subtraction algorithms. Lesion-size accuracy is already an area of potential concern in software that produces 3-D endoluminal views. Moreover, size is the best indicator of a lesion's clinical importance, so accuracy is essential for reporting and patient management.
Size distortions could occur in the form of pseudoenhancement of a structure due to the high density of material surrounding it, Zalis said "e.g., a polyp surrounded by tagged feces." To test their hypothesis, the group conducted another study using a phantom built specially to address pseudoenhancement in tagged material.
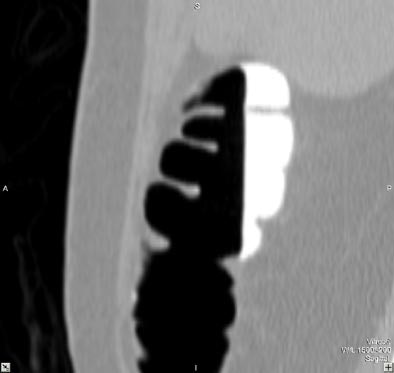 |
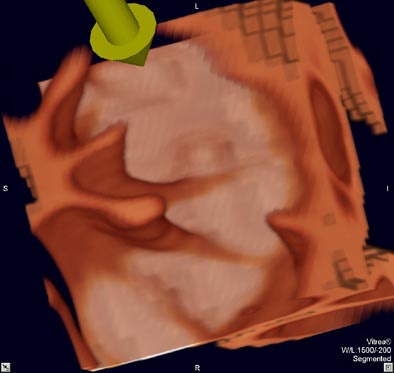
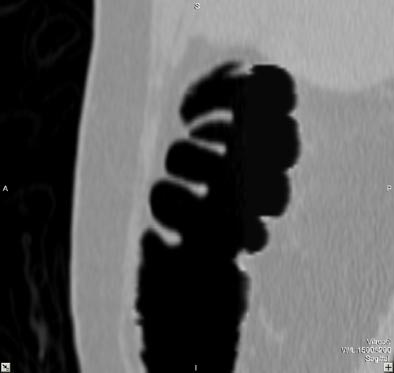
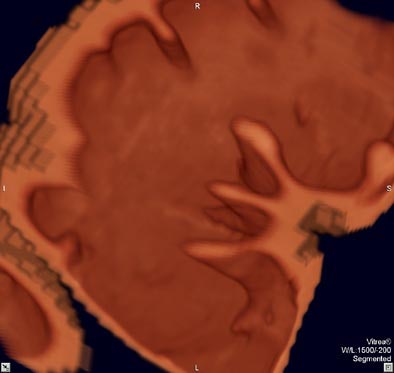
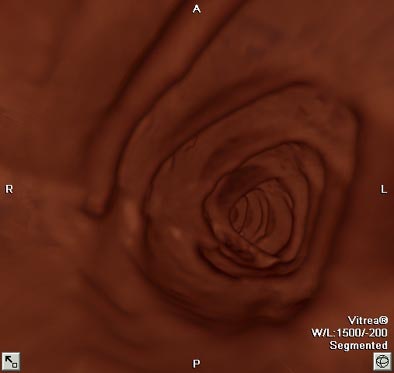
| Virtual colonoscopy images of an asymptomatic 56-year old woman who ingested small aliquots of nonionic iodinated contrast, without dietary restrictions, prior to virtual colonoscopy. The evening before the exam, the patient ingested a half dose of mild cathartic, markedly reduced from standard regimens. Images top to bottom: Sagittal view of cleansed colon following the preparation; corresponding cutaway view; volume-rendered endoluminal views of the same region demonstrate opacificed material in the colon. Further below, the same set of images after the subtraction software has removed opacifying material and reconstructed a natural appearing colonic mucosa, as seen in sagittal; cut-away; and endoluminal (fly-through) views. The green arrow points to some of the contrast which is layering in the dependent portion of the colon. All images courtesy of Dr. Michael Zalis. |
 |
 |
 |
 |
 |
"The impetus for the study was to define an operational range of contrast density we should shoot for in all our upcoming minimal prep work," Zalis told AuntMinnie.com. "If the stuff is too dense, it might artificially decrease the measured size of lesions, and if it's not dense enough, the subtraction would not be clean."
The study had to be done in a phantom, since it required scanning and rescanning the same polyps over and over again to test the whole range of contrast densities, he said.
So test they did -- a whole range of stool-tagging regimens in 21 scans -- with the resulting mean contrast density ranging from 200 HU up to 800 HU. Following imaging with CT, subtraction and mucosal reconstruction algorithms were implemented on a DICOM-compliant software application that was developed at the institution and written in an existing programming system (Matlab, Natick, MA).
"To summarize, we found no statistically significant differences between subtracted lesions and control in comparison to a reference standard when the concentration of contrast was below 550 HU. And above that, when the density got too high, then there was artifact that resulted in small but statistically significant changes in polyp size," Zalis said.
For example, after electronic digital subtraction of the phantom "fecal material," a polyp measuring 19 mm on the reference standard grew smaller as the density of the surrounding prep increased.
"Moving to a 300-HU prep (there is) artificial elevation in the density of the polyp due to the fact that it's surrounded by this high-density material," he said. "And as a result, in this particular example we measured it as 18.7 mm -- a statistically significant change. Moving up to a much higher (contrast) concentration at 360 HU, you can see there's a lot of streak artifact and pseudoenhancement of this lesion...We measured this (polyp) as 17.4 mm and averaged it over a group of 21 polyps in this setting. That is a statistically significant change (in size). Small but significant."
The study has been submitted for publication, and a follow-up study is in progress, he said.
"This is a big discussion," he said. "I think the current data are preliminarily encouraging for the use of minimal preparation techniques. I think we have some further work to do in terms of optimizing the (minimal) prep in part so that more of the time we get that excellent homogeneous, no air, semi-liquid opacified material."
The group is also considering the addition of a stool softener in order to reduce the water content slightly, and produce more-homogeneous tagging. Then, he said, "we'll finally be able to rigorously validate all of these data and produce a much better trial. With this I think patient compliance will improve as well."
By Eric BarnesAuntMinnie.com staff writer
March 8, 2004
Related Reading
German group optimizes barium-sulfate tagging in MR colonography, January 22, 2003
Copyright © 2004 AuntMinnie.com