A deep-learning (DL) model can automatically measure myocardial blood flow on CT scans to help diagnose myocardial ischemia, according to a study published April 29 in Radiology.
The finding is from a group in China at Shanghai Jiao Tong University that first developed the model and then validated it in a prospective cohort of 660 participants who presented with chest pain at three hospitals.
“Applying this DL model into clinical practice may facilitate the clinical workflow of ischemia imaging, provide a powerful tool for the precise quantification of ischemic burden, and optimize prognosis assessment,” noted corresponding author Jiayin Zhang, MD.
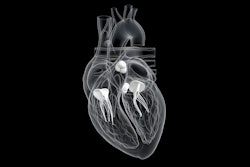
Myocardial ischemia occurs when blood flow to the heart muscle is obstructed by a partial or complete blockage of a coronary artery by plaque buildup. If the plaques rupture, patients may experience major adverse cardiovascular events (MACE), such as heart attack.
Dynamic CT myocardial perfusion imaging (MPI) is a useful approach for detecting myocardial ischemia based on measuring myocardial blood flow, yet there are no techniques available that can precisely quantify ischemic myocardial volume percentages, which is a key guiding treatment strategy, the authors wrote.
In this study, the group developed a DL model that fully automates the quantification of myocardial blood flow (MBF) and ischemic myocardial volume (IMV) percentages and explored its prognostic value.
 Representative images from diagnostic analysis of deep learning (DL)-based CT myocardial perfusion imaging (MPI). (A-D) Representative images in a 51-year-old woman with stable angina at presentation. (A) Curved planar reformation and (B) three-dimensional maximum intensity projection images show severe stenosis of the opening left anterior descending artery (arrow). (C) Fractional flow reserve (FFR) determined with invasive coronary angiography helps confirm that there was no hemodynamic significance of the opening left anterior descending artery lesion (arrow). (D) Dynamic CT MPI provided functional information to identify hemodynamically significant stenosis with reference to invasive FFR. Myocardial blood flow (MBF) derived from DL-based CT MPI revealed the absence of decreased myocardial perfusion of the left anterior descending artery territory (the areas outlined in black represent the myocardium subtended by the left anterior descending stenosis, and the color bar is a graphical scale that maps MBF ranges). (E-H) Representative images in a 62-year-old man with exertional chest pain at presentation. (E) Curved planar reformation and (F) three-dimensional maximum intensity projection images show moderate stenosis of the middle left anterior descending artery (arrow). (G) FFR determined at invasive coronary angiography helps confirm that the middle left anterior descending lesion was hemodynamically significant (arrow). (H) Dynamic CT MPI provided functional information to identify hemodynamically significant stenosis with reference to invasive FFR. DL-based CT MPI showed a reduction in MBF within the middle and basal anterior wall of the left anterior descending artery territory (the areas outlined in black represent the myocardium with decreased perfusion, and the color bar is a graphical scale that maps MBF ranges). MBFDL = MBF derived from the DL model.Radiology and the RSNA
Representative images from diagnostic analysis of deep learning (DL)-based CT myocardial perfusion imaging (MPI). (A-D) Representative images in a 51-year-old woman with stable angina at presentation. (A) Curved planar reformation and (B) three-dimensional maximum intensity projection images show severe stenosis of the opening left anterior descending artery (arrow). (C) Fractional flow reserve (FFR) determined with invasive coronary angiography helps confirm that there was no hemodynamic significance of the opening left anterior descending artery lesion (arrow). (D) Dynamic CT MPI provided functional information to identify hemodynamically significant stenosis with reference to invasive FFR. Myocardial blood flow (MBF) derived from DL-based CT MPI revealed the absence of decreased myocardial perfusion of the left anterior descending artery territory (the areas outlined in black represent the myocardium subtended by the left anterior descending stenosis, and the color bar is a graphical scale that maps MBF ranges). (E-H) Representative images in a 62-year-old man with exertional chest pain at presentation. (E) Curved planar reformation and (F) three-dimensional maximum intensity projection images show moderate stenosis of the middle left anterior descending artery (arrow). (G) FFR determined at invasive coronary angiography helps confirm that the middle left anterior descending lesion was hemodynamically significant (arrow). (H) Dynamic CT MPI provided functional information to identify hemodynamically significant stenosis with reference to invasive FFR. DL-based CT MPI showed a reduction in MBF within the middle and basal anterior wall of the left anterior descending artery territory (the areas outlined in black represent the myocardium with decreased perfusion, and the color bar is a graphical scale that maps MBF ranges). MBFDL = MBF derived from the DL model.Radiology and the RSNA
The study included three cohorts of patients, two retrospective and one prospective, who underwent dynamic CT MPI as well as coronary CT angiography (CCTA), a noninvasive method for excluding obstructive coronary stenosis in patients with an intermediate risk of disease.
The DL model was developed in cohort 1 (training set, 211 patients; validation set, 57 patients; test set, 90 patients). The researchers compared the model’s performance in calculating MBF to a manual method using commercially available software (VPCT body, Siemens Healthineers), with the model achieving “excellent agreement” with the manual technique.
Next, in cohort 2 (90 patients with 116 vessels with stenosis), they evaluated the diagnostic performance of MBF derived from the DL model for predicting myocardial ischemia based on area under the receiver operating characteristic curve (AUC). Here, the model showed higher diagnostic performance (AUC, 0.96) than CT-derived fractional flow reserve (AUC, 0.88) and CCTA-derived diameter stenosis (AUC, 0.8).
Finally, in cohort 3, a total of 660 participants were followed up for at least two years. MACE occurred in 94 participants (14.2%), and “hard” MACE (cardiac death, nonfatal myocardial infarction) occurred in 26.
A multivariable Cox regression analysis revealed that DL-based IMV was an independent predictor for MACE, indicating that for every 10% increase in IMV, the risk of MACE occurrence rose by approximately 20%.
“In this study, we successfully developed and validated a DL model for fully automated postprocessing of dynamic CT MPI,” the authors wrote.
Ultimately, compared with nuclear or cardiac MRI perfusion imaging, dynamic CT MPI combined with CCTA is a “one-stop shop” imaging modality that can reveal coronary atherosclerosis and myocardial ischemia, the authors noted. However, to date, it has remained unclear whether AI techniques can enhance the quantification of MBF, enable accurate diagnosis of myocardial ischemia, and improve risk stratification of coronary artery disease.
“To the best of our knowledge, this is the first AI approach dedicated to the analysis of CT MPI data,” the group wrote.
The full study is available here.