U.S. radiologist Dr. Gautham Reddy returned to the city of his birth -- Hyderabad -- to provide IRIA attendees with an overview of the latest techniques in cardiac imaging with MRI and CT.
Reddy was born in Hyderabad in 1963, but his family moved to the U.S. in 1967. He is currently assistant professor of radiology and associate director of the residency program at the University of California, San Francisco.
In his IRIA presentation, Reddy discussed how ischemic heart disease is the leading cause of mortality in developed countries: In the U.S., treating heart disease costs around 1.5% of the country's gross domestic product, or almost $500 billion a year.
Until recent years, the rapid motion of the heart made it difficult to use CT and MRI for cardiac assessment. New technological advances, however, have enabled both modalities to carve out niches effective tools for imaging the heart, in particular the coronary arteries.
Imaging professionals are turning to CT and MRI as an alternative to cardiac catheterization, the gold standard for heart imaging. Some 40% of cardiac catheterizations turn out to be normal, unnecessarily putting patients at risk of morbidity or mortality. "Why do so many invasive tests on patients who have normal coronary arteries?" Reddy said. "We need a noninvasive way to image coronary arteries."
Cardiac CT
Two types of CT technologies are available for cardiac imaging: electron-beam computed tomography (EBCT) and multislice CT (MDCT), Reddy said. EBCT's advantage is its fast temporal resolution of 70-100 ms. EBCT also offers lower radiation dose than MDCT.
However, MDCT technology has better spatial resolution and is far more widely available than EBCT, Reddy said, and newer MDCT scanners with more slices per rotation and sub-millimeter resolution are making MDCT even more competitive. For example, 16-slice scanners can achieve temporal resolution of up to 108 ms for some patients, he said.
What are the best applications for cardiac CT? The technology has demonstrated the highest value for three main applications:
- Coronary angiography.
- Coronary calcium scoring.
- Characterization of coronary plaque.
Coronary CT angiography (CTA) has attracted perhaps the most attention because it is a noninvasive means of imaging coronary stenosis, Reddy said. A recent meta-analysis of coronary CTA studies found the technology to have a sensitivity of 84%, a specificity of 91%, and a negative predictive value of 96%. The high negative predictive value in particular is crucial, he said: it implies that if you do a CTA of the coronary arteries, and it is normal, then you can rule out coronary artery disease.
Coronary CTA can be confounded, however, under some conditions. These include motions artifacts in patients with heart rates faster than 65 beats per minute, cardiac arrhythmias, and dense coronary calcium with an Agatston score great than 100. Beta blockers are often used to slow down the heart rate prior to multislice CTA. Coronary stents can also cause artifacts on both CT and MRA, although preliminary research has indicated that the evaluation of coronary stenosis is possible in the presence of a stent.
Coronary calcium scoring was once the exclusive domain of EBCT, but MDCT scanners are showing increasing utility in this area. There is still some confusion in terms of the best technique to use to measure calcium score -- there have been some discrepancies reported between Agatston scores collected by EBCT studies and those of MDCT scans. New scoring methodologies have been proposed, such as one that relies on calcium volume and mass.
Coronary plaque characterization is becoming increasingly important as investigators realize that plaque stability and the risk of plaque rupture are major factors in whether a patient suffers a cardiac event. Cardiac CT may be able to tell the difference between lipid, fibrous, and calcific plaque based on CT density values.
"Soft plaque is the primary cause of sudden coronary events," Reddy said. "Evaluation of the presence, location, and characterization of soft plaque may be an ideal way of evaluating patients at risk of a coronary event. If we do soft plaque CT we might want to do coronary CTA at the same time."
Cardiac CT also has utility in the following applications:
- Characterizing mitral valve thickening, mitral valve calcification, and mitral annulus calcification.
- Characterizing aortic valve morphology, aortic annulus diameter, and aortic valve calcification.
- Confirming endocarditis by visualizing valvular vegetation.
- Mapping the coronary venous system to expedite venous cannulation.
- Measuring left and right ventricular volumes, ejection fraction, and left ventricular mass.
- Imaging work-up of congenital heart disease by adding its strength in 3-D spatial resolution to data gathered by other imaging modalities.
Cardiac MRI
Like CT, MRI can perform studies of cardiac anatomy. But the modality has the added advantage of being able to also provide information about myocardial perfusion, ventricular function, and myocardial viability
Coronary MRA has been on the cusp of routine clinical use for the past 15 years, and that's still true today, Reddy said. Multicenter studies have demonstrated good marks for three-vessel disease, but false-positives are a problem in overall coronary imaging: one study found a sensitivity of 94%, specificity of 45%, and negative predictive value of 82%.
Both CTA and MRA have similar sensitivity and specificity ratings in published studies. CTA has an advantage in that it is fast, simple, and easily reproducible, and Reddy said he believes that you're more likely to get a good-quality diagnostic image with coronary CTA than MRA because MR is highly variable. CTA is also useful for imaging calcium and soft plaque, which can help predict which patients are at risk of heart attack.
MRA has the edge in its lack of ionizing radiation or iodinated contrast agent, which makes possible multiple imaging attempts (this can be a double-edge sword, though, Reddy believes). Coronary flow measurements are also possible.
A shortcoming of both techniques is that they are limited to providing anatomic information, and both lack high specificity. However, they can be used in combination with functional techniques such as perfusion to improve specificity, Reddy said.
MR perfusion
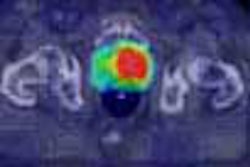
MR perfusion imaging is typically first-pass imaging with a gadolinium contrast agent and a pharmacological stressor (pharmacological stressors are more commonly used rather than exercise stress due to the difficulty in locating exercise equipment in the scanner).
Fast imaging protocols are required to detect regional myocardial perfusion during the first pass of the contrast medium; images need also be acquired at multiple levels in the short-axis or long-axis planes. Fast gradient-echo T1-weighted sequences have a high signal-to-noise ratio and good image contrast, although temporal resolution is a limitation. Hybrid echo-planar imaging (EPI) is a good compromise between single-shot EPI and gradient-echo sequences, especially when used in conjunction with sensitivity encoding (SENSE) parallel imaging sequences.
Studies indicate that MRI performs better than SPECT and similarly to PET in cardiac perfusion, Reddy said. MRI has an advantage over PET in that PET is not widely available and is more expensive.
MR functional imaging
With functional imaging, MRI is used to assess wall motion and how well the heart is pumping. This is also conducted with a pharmacologic stressor, and studies indicate that dobutamine is the best choice for wall-motion studies, Reddy said.
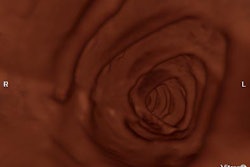
Cine loops of the heart are acquired with a gradient-echo or segmented k-space turbo gradient echo sequence. The arrival of steady-state sequences has resulted in shorter scan times and better image quality.
Echocardiography with dobutamine is often used for wall-motion studies, but the modality is highly operator-dependent and studies indicate that MRI can offer superior image quality, supporting its use as an adjunct to echo to detect ischemic heart disease in patients with poor echo image quality. MRI's image quality and spatial resolution provide better delineation of the endocardial border, leading to more accurate assessment of wall thickness and wall thickening.
Nagel demonstrated an increase in sensitivity and specificity from 74% and 70%, respectively, for dobutamine echocardiography to 86% and 86% for dobutamine MRI. Test accuracy also improved, with dobutamine echo rating 73% and dobutamine MRI 86%.
With myocardial viability imaging of the left ventricle, the main goal is to find living tissue, Reddy said. If the tissue isn't viable, then therapeutic interventions such as coronary artery bypass grafts, angioplasty, or stents aren't necessary. MRI can help determine which patients would benefit from stents or surgery.
MRI myocardial viability imaging is based on the principle that an area suffering from myocardial infarct display hyperenhancement 10-15 minutes after contrast is applied. Areas of the heart that are at risk but not infarcted do not hyperenhance -- therefore, the tissue is still viable. "This is no reason to do treatment (in patients with white areas). If there are dark areas the patient can benefit from revascularization," Reddy said.
PET is the gold standard for myocardial viability, but MRI can identify scar more frequently than PET.
Reddy concluded by predicting that MRI would eventually progress to the point where global heart assessments with the modality became a routine clinical procedure, while perfusion and functional viability techniques may be developed for CT.
Following his presentation, a panelist asked Reddy if he had seen patients go straight into surgery based solely on MRI or CT findings. Reddy said that coronary angiograms are always ordered prior to surgery, but that MRI or CT can help screen normal patients from undergoing a diagnostic angiogram.
By Brian Casey
AuntMinnie.com staff writer
March 12, 2004
Related Reading
MRI useful in detecting thrombus in left atrial appendage, October 20, 2003
MRI useful in detecting complicated carotid plaques, June 10, 2003
CTA, MRA advance aneurysm diagnosis and follow-up, April 30, 2003
CMS sets date for expanded MRA coverage, April 17, 2003
Transthoracic ultrasound detects adequate reperfusion after anterior MI, October 30, 2002
Copyright © 2004 AuntMinnie.com