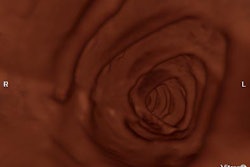
These days it seems that every radiology department is trying its hand at virtual colonoscopy, and publishing its results. The steadily rising volume of data published in single-institution studies has been a boon for those wanting to learn more about the technique. On the other hand, wide variations in the quality and consistency of techniques used have often made it impossible to compare one study to the next.
In a recent editorial published in Radiology, Dr. Abraham Dachman from the University of Chicago and Dr. Michael Zalis from Massachusetts General Hospital in Boston present their case for improved standardization of study and reporting methods (Radiology online, February 10, 2004).
"Many of the questions now being posted for CT colonography (virtual colonoscopy) require evaluation in large multicenter trials, few of which have had their results published," they wrote. "In the meantime, many important questions are answerable in the synthesis of the findings from single-institution studies. However ... meta-analysis of these smaller investigations has been limited by the variability in the acquisition, reporting, and analysis of data."
The standards they propose, many of which are already in common use among top VC researchers, will render meta-analyses more valuable while giving radiologists a standard against which they can measure their own progress, Dachman and Zalis wrote.
Exams and reporting
In order to perform VC with a drier colon, the researchers recommend the use of a saline cathartic (sodium phosphate or magnesium citrate preparation) rather than colonic lavage with polyethylene glycol, unless the lavage is medically indicated (e.g., sodium is contraindicated). Scan times should be 30 seconds or shorter in order to minimize respiratory motion, and overlapping breathhold acquisitions are discouraged as "less desirable for a seamless three-dimensional endoluminal fly-through."
Multidetector-row CT is recommended over single-slice, as is "the use of (a) collimation of 3 mm or less and (b) overlapping sections at an interval that is two-thirds or less of the collimation," the authors wrote.
Virtual colonoscopy investigators should take care to report the prevalence of polyps and masses in the cohort, sensitivity both by patient and by polyp, and specificity, positive and predictive negative values, each stratified by lesion size and location. Histologic findings and a detailed description of the reporting methods should be included in the study.
Is the cohort at an average or high risk of polyps? What is the symptomology of the high-risk patients? All this information should be detailed in the study Dachman and Zalis wrote. Also, newly recognized risk factors and disease associations should be sought.
The by-patient analysis is the most clinically salient measure of the exam's effectiveness, because it gauges the number of patients correctly referred for conventional colonoscopy after a positive exam, the authors wrote. However, the by-polyp analysis remains the best measure of virtual colonoscopy's capabilities.
"Optical colonoscopy is not a perfect reference standard; with optical colonoscopy, as many as 25% of diminutive polyps (< 5 mm in diameter) and 6% of polyps 1 cm and larger may be missed," they wrote. "If there is a discrepancy between the findings from (VC) and optical colonoscopy in a clinical setting, this discrepancy should be evaluated on a case-by-case basis."
Size matters
Because lesion size is directly related to the possibility of its being cancerous, size matters. The caliper tool is ideal for measuring polyps in endoscopy, but is rarely used, the authors wrote. Using forceps instead is fine, as long as the tool is held as close as possible to the lesion. The lack of blood flow and the cautery effect of resected polyps make measurements of their size unreliable, and soaking in formalin shrinks the lesion further. So in vivo measurements are best for conventional colonoscopy, but in any case the measurement method should be specified.
For virtual colonoscopy, 2-D multiplanar images provide the most accurate lesion-size measurements, Dachman and Zalis stated. They further recommended the reporting of polyps in size categories such as 5-9 mm, adding that masses 4 mm and larger be reported separately from polyps.
"We recognize that some lesions are oval and perhaps measured more easily on three-dimensional endoluminal views," they wrote, "but (3-D) measurement of size is subject to potential distortion, and this topic deserves further research. We propose that for standardization, the largest single dimension should be reported for a given lesion, analogous to the 'response to treatment in solid tumors criteria.'"
The authors further recommended that sensitivity, specificity, and positive and negative predictive values should be restated for a variety of polyp-size cutoffs such as 7, 8, or 9 mm.
Optical or conventional colonoscopy has a necessarily imprecise relationship with mass location, since there is "little direct extraluminal reference with which to correlate the position of the endoscopy," the authors noted, adding that colon stretching during the exam subjects it to potential overestimation of the distance between the rectum and the lesion.
"Because many trials forbid unblinding of the researchers until the end of the trial, we suggest that investigators further document the location of the lesion at endoscopy by determining the distance from the anal verge and by acquiring still images of each lesion," they wrote.
Things are easier in virtual colonoscopy, of course, and the authors believe that investigators should estimate the segmental location of each lesion if possible. They also recommend the reporting of six rather than eight segments, including the rectum, sigmoid colon, descending colon, transverse colon, ascending colon, and cecum.
"We suggest avoiding 'hepatic flexure' and 'splenic flexure' as separate segments," they wrote. "Although the location of the flexures is usually well defined for the radiologist, there is no corresponding clear transition point between the flexures and the adjacent colonic segments for the endoscopist."
Researchers should also provide histologic data including that of hyperplastic polyps, adenomatous polyps, and carcinomas, they said, because most of the time carcinomas appear to arise from benign adenomas.
"Hyperplastic polyps are not considered premalignant, although there are emerging reports that hyperplastic polyps (especially when located proximally) may be a precursor of malignancy through a rapidly progressive (though as yet poorly understood) mutator pathway," Dachman and Zalis wrote.
Synchronicity, morphology, and technique
In a nod to the power of the by-patient analysis, the authors suggest that radiologists can save time and fatigue by avoiding a detailed search for a synchronous lesion once another lesion has already been detected, since the patient will likely be referred for optical colonoscopy at that point anyway. Radiologists should always examine the entire colon, however, as optical colonoscopy has a miss rate estimated at 6% for 10-mm lesions.
The authors suggested standardized descriptions of lesions as pedunculate, or mushroom cap-shaped with a stalk; sessile lesions are broader, mesa-shaped lesions attached to the colonic wall; and flat lesions are 2-mm or less higher than the surrounding mucosa. Each type may have a different risk of harboring carcinoma.
Flat lesions remain especially difficult to detect in virtual colonoscopy, they noted; moreover, their high degree of dysplasia suggests that flat lesions may not follow the usual time course for the adenoma-carcinoma sequence.
"Several investigators have suggested that hyperplastic polyps may flatten and may be less conspicuous in well-distended or overdistended colons," Dachman and Zalis wrote. Flat lesions should be further categorized as either infiltrative, those with no perceptible raised component, or rising at least a few millimeters into the colon.
Follow-up data that changes the ground truth should be reported separately from the original results, they suggested, and investigators should take care to report the reasons for each false-positive or false-negative result. As "low-dose" is a nebulous term, Dachman and Zalis suggested that researchers include the precise imaging protocol for each study.
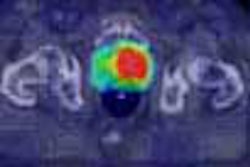
And they recommend that investigators indicate the precise reading conditions for observers, including their experience levels, the software and hardware platforms used, single versus dual-monitor reading, mouse versus button-control navigation, and automated versus manual fly-through of 3-D endoluminal reconstructions. The number of nondiagnostic studies should be reported. They suggested that the stool opacification method be reported, as well as the CAD algorithm when applicable, preferably as a "second opinion."
"Little head-to-head comparison has been made of these different viewing factors, and complete reporting of them will assist in retrospective analysis of their efforts," they wrote.
Researchers who use confidence scales can benefit by gauging quality of distension, residual fluid, or residual stool on a five-point scale, for example. The study should indicate whether their conclusions are based on independent reading or consensus. Independent multiple-observer studies are preferred, the authors wrote.
"In the long term, we must develop guidelines to link CT colonographic results to recommendations for patient care," Dachman and Zalis wrote. "(Virtual colonoscopy) will force us to address the question: what is the appropriate management for lesion in the size categories listed previously? We must develop standard recommended intervals between examinations that take patient risk stratification and examination performance data into consideration."
The largest and most consistent pool of data that researchers can possibly create is the one that will help answer these questions most readily, they concluded.
By Eric BarnesAuntMinnie.com staff writer
March 17, 2004
Related Reading
Tailor insufflation technique to the patient, says VC researcher, January 30, 2004
Experience sharpens role of IV contrast-enhanced VC, January 19, 2004 Thinner collimation improves polyp detection -- sometimes, November 26, 2003Researchers settle on 'best' CT protocol for multislice virtual colonoscopy, September 25, 2003
Copyright © 2004 AuntMinnie.com