A negative chest CT scan correlates with a very low risk of pulmonary embolism in subsequent months, according to researchers from Ireland. In a study published in the American Journal of Roentgenology, radiologists from the Mater Misericordiae Hospital in Dublin also found that MDCT pulmonary angiography determined the underlying causes of patients' signs and symptoms most of the time.
"CT pulmonary angiography has increasingly become the tool of choice in the diagnosis of pulmonary embolism, (yielding) sensitivity of 60%-100% and specificity of 78%-100% in the diagnosis of pulmonary embolism," wrote Dr. Eoin Kavanagh and colleagues (AJR, February 2004, Vol.182:2, pp. 499-504).
Owing to multislice scanners and 1.25-mm reconstructions, better visualization of subsegmental vessels is likely to continue improving diagnostic accuracy and perhaps reduce the rate of subsequent PE, they wrote. And because of the dangers of administering anticoagulant therapy following a negative scan, the study could bolster a clinician's decision to go therapy-free in such cases.
Previously, Swensen et al had concluded that withholding anticoagulation therapy following a negative exam was probably a safe therapeutic option, having detected PE in only 0.5% of such patients within three months after MDCT (Mayo Clinic Proceedings, February 2002, Vol. 77:2, pp. 130-138).
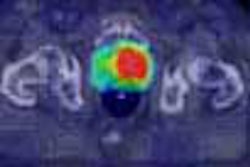
In the Irish study, 102 consecutive patients with suspected pulmonary embolism underwent MDCT pulmonary angiography on a four-slice Somatom Volume Zoom scanner (Siemens Medical Solutions, Malvern, PA). The MDCT cohort came from a total of 290 patients with suspected PE, 188 of whom were referred for ventilation-perfusion scans, at the discretion of clinicians.
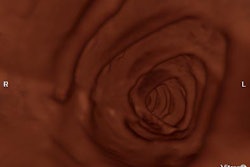
Following a bolus injection of 120 mL of 300 mg I/mL of iodinated contrast at 3 mL/sec, MDCT images were acquired using a slice thickness of 1.25 mm and slice interval of 1.2 mm. Images were reviewed on a Siemens MagicView workstation by two radiologists and the results decided by consensus.
Based on the criteria of Tillie-Leblond, "the presence of an endoluminal filling defect on CT pulmonary angiogram was considered diagnostic of pulmonary embolism," the authors wrote. The team also graded scan quality on a scale of 1 to 4, 4 being nondiagnostic. Patients graded 3 and 4 were recommended to undergo further imaging to exclude PE embolus as a cause of symptoms. Additional abnormalities that may have accounted for the patient's symptoms were also noted.
Eighty-five patients (ages 20-94) had no CT sign of PE and became the study group. The exams of 64/85 patients (75%) were graded 1 (sufficient to exclude emboli to the subsegmental arterial level), while 18 exams (21%) were graded 2 (adequate to exclude emboli to the segmental level). Three exams were grade 3 (PE excluded only at main and lobar levels), and none were rated 4.
Sixty-four patients (75%) had additional findings, including 10 patients (12%) with pleural effusion, 15 (18%) with consolidation, 18 (21%) with emphysema, four cases of bronchogenic neoplasm (5%), seven (8%) with segmental or lobar atelectasis, four (5%) with pulmonary fibrosis, and two (2%) with floral mediastinal adenopathy, and one each with pulmonary tuberculosis and arteriovenous malformation.
Seventeen (20%) of the patients died before clinical follow-up; none with documented PE. At follow-up, 6/68 living patients were receiving anticoagulant therapy, including two for cerebrovascular disease, two for deep venous thrombosis, and two for pulmonary embolism, the authors wrote (these patients were not excluded from follow-up because of their numbers -- they constituted 9% of the cohort).
Follow-up included clinical review by telephone (66 patients), interview with a primary care or referring physician in six patients, chart review in 26 patients, review of autopsy reports in five patienets, or review of death certificates in 12, the authors wrote.
The authors defended their decision to perform clinical follow-up rather than pulmonary angiography, noting that recent studies have questioned the accuracy of pulmonary angiography for the detection of isolated subsegmental emboli.
"It is accepted that pulmonary embolism occurring within three months of a CT pulmonary angiography that showed no signs of (PE) most likely indicates a false-negative examination," the authors wrote. "This approach may miss small emboli that do not present with patient symptoms, but such emboli are unlikely to be clinically significant if no evidence of recurrent thromboembolic disease has been noted three months or longer after initial presentation."
Subsegmental pulmonary emboli were seen in one patient who underwent follow-up ventilation-perfusion scanning within three weeks after MDCT -- in an exam graded 1. The case was deemed a false false-negative, as the subsegmental pulmonary emboli could be seen retrospectively on CT in the patient, who had multiple comorbidities. Thus, the risk of PE following negative MDCT was 1%, in line with previous studies showing the NPV of MDCT pulmonary angiography to be 98% to 100%.
"Unlike ventilation-perfusion scanning, CT pulmonary angiography showed a cause for symptoms in 76% of patients in our study; 47% of these findings were not suspected from findings on chest radiography," they wrote.
The results confirmed that MDCT pulmonary angiography in patients with no signs of pulmonary embolism correlates with a very low risk of subsequent clinically significant pulmonary embolism, according to the authors.
"This finding is important in further treatment of these patients because unnecessary referral for pulmonary angiography or treatment with anticoagulation can result in serious complications," Kavanagh and colleagues wrote. "Anticoagulation treatment with warfarin is associated with fatal hemorrhage in 0.4% and nonfatal major hemorrhage in 6% of patients."
By Eric BarnesAuntMinnie.com staff writer
March 22, 2004
Related Reading
Volumetric capnography points to pulmonary embolism, March 17, 2004
CT assessment of pulmonary embolus predicts prognosis, March 16, 2004
Combined test strategy safely detects pulmonary embolism in outpatients, March 11, 2004
Troponin I test adds to prognostic value of echo in acute pulmonary embolism, October 27, 2003
D-dimer testing can eliminate need for ultrasound in patients with suspected DVT, September 25, 2003 High pitch, thin sections can optimize MDCT protocols, August 22, 2003 Copyright © 2004 AuntMinnie.com