
CT/MRI fusion is a waste of time for postbrachytherapy imaging of the prostate, say researchers from Boston and Vienna. Not only does contrast-enhanced MRI detect seeds nearly as well as CT, they say, but MRI’s superior soft-tissue contrast properties often make it the only way to tell whether seeds have migrated outside the organ.
Seed dislocation following brachytherapy may increase the risk of urinary, erectile, and anorectal complications, and could pose significant additional risks when seeds migrate to the heart and lungs. To date, however, there have been no reports of adverse reactions to pulmonary embolization of the radioactive seeds, which has been reported to occur in 10%-20% of brachytherapy patients.
The MR/CT comparison was performed by lead investigator Dr. Nicolas Bloch from Beth Israel Deaconess Medical Center in Boston, Dr. Klaus Kubin from the University of Vienna in Austria, and their colleagues on both sides of the Atlantic. Kubin presented the preliminary results of the ongoing study at the 2004 European Congress of Radiology, while Bloch followed up in a telephone interview with AuntMinnie.com.
"The American and European brachytherapy societies recommend CT imaging to evaluate post-implant migration," Kubin said in his presentation. However, even though CT is useful for identifying seeds, its poor soft-tissue contrast often makes it impossible to delineate the anatomy of the prostate gland and surrounding structures, he said. As a result, it is often impossible to determine the precise location of seeds visualized in CT exams.
The study compared the value of contrast-enhanced T1-weighted MRI, T2-weighted MRI, and CT for intra-and extraprostatic seed distribution. About four weeks post-brachytherapy, 15 patients underwent prostate imaging on a 1.5-tesla MRI scanner (Siemens Medical Solutions, Malvern, PA) with a combined surface and endorectal coil. Within the following week, CT images were acquired on a Siemens single-slice helical CT scanner.
MRI transverse images were acquired seven minutes after administration of gadolinium-DPT using two protocols:
- T2-weighted TSE (4000/83/5 min. 24 sec, FOV 160)
- T1-weighted 3-D FLASH GRE (8.1/4/1 min. 35 sec., FOV 160)
Non-contrast CT images were acquired using 5-mm collimation, 130 kVp, 110 mAs, pitch 1.5.
"We analyzed the intra- and extraprostatic seed distribution, especially in the central gland and peripheral zone and periureter, and extraprostatic and periprostatic tissue," Kubin said. "We looked at the...penile bulb, the rectal wall, the urinary bladder base, the seminal vesicles, and the neurovascular bundles."
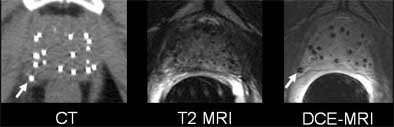 |
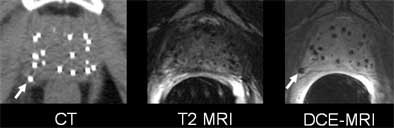
| Wayward brachytherapy seeds are well visualized, and better localized, in the contrast-enhanced MRI (the "D" in DCE-MRI stands for "dynamic," which is not necessary to optimize seed visualization, according to the authors). In patient 1 (top), a brachytherapy seed has migrated to the neurovascular bundle. In patient 2 (below), CE-MRI shows a seed that has lodged in a seminal vesicle, but cannot be localized in CT image at left. In patient 3 (bottom), the migration of seeds to the penile bulb is readily visualized on contrast-enhanced ("CE") MRI, lower right. All images courtesy of Dr. Klaus Kubin. |
 |
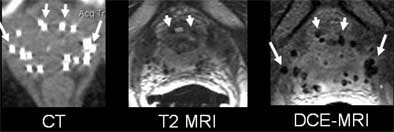 |
According to the results, the T1-weighted GRE sequence localized 92% of the seeds overall (with per-patient accuracy ranging from 87%-99%), 14% of which were periprostatic. Twenty-five percent of the seeds were located in the neurovascular bundle, and 4% in the seminal vesicles.
T2-weighted MRI localized 78% of the seeds overall (range, 74%-86%), including 12% in periprostatic distribution, which was diagnosed more accurately on the T2 images. Twenty-four percent were found in the neurovascular bundle and 3% in the seminal vesicles, Kubin said.
CT won the sensitivity race, locating 97% of the seeds (range, 95%-100%). Two percent were suspected to be extraprostatic; however, the group was unable to assign the seeds to specific periprostatic structures.
The group concluded that T1- and T2-weighted MR were both more accurate for postbrachytherapy seed distribution than CT.
"The main idea is that the prostate takes up contrast media in general, not only the cancer, so if you wait long enough (up to 11 minutes after injecting contrast) the whole prostate is contrast enhanced," Bloch said. "But the seeds, of course, you see as voids because there is no contrast uptake. So if you use high-spatial-resolution MRI, no matter if it’s T2- or T1-weighted contrast enhanced, you see very nicely the prostate, the prostate capsule, and the neurovascular bundle, the penile bulb, and the rectal wall, but until now you couldn’t see the seeds."
Bloch said that he and his colleagues in Vienna have found through experience that CT’s inability to delineate the anatomy is not improved by the use of thinner collimation or MDCT scanners with as many as 16 detectors. In fact, he said, some researchers have reported that very thin CT slices can lead to the problem of double-counting seeds. As for CT/MR fusion, he said that exquisitely performed studies have demonstrated that it works, but the technique is both time-consuming and complicated.
"You don’t need fusion," Bloch said. "This is the message."
Lately the Boston researchers have been working on a study that combines MR imaging of the prostate with an automated seed-detection application originally developed for CT. Results so far have been excellent, he said.
An audience member at the ECR presentation noted that contrast media adds about 100 euros to the cost of the MRI exam. Kubin said that for now, CT is still used in his department because it's cheaper.
By Eric BarnesAuntMinnie.com staff writer
May 19, 2004
Related Reading
Point/counterpoint: Prostate cancer researchers battle over treatment options, May 14, 2004
Urinary flow tied to prostate cancer brachytherapy outcome, April 2, 2004
New fusion method joins MR and CT in prostate cancer therapy planning, March 5, 2004
Use of prostate brachytherapy has risen dramatically in U.S., November 17, 2003
Radioactive seed migration common after prostate brachytherapy, April 29, 2002
Copyright © 2004 AuntMinnie.com




















