
An important new study from Italy bodes well for virtual colonoscopy. In fact, it's good news for anyone who might be willing to undergo colorectal cancer screening if it weren't for the uncomfortable bowel prep.
Researchers from the University of Rome "La Sapienza" found high sensitivity and specificity in a low-dose prepless virtual colonoscopy study of 203 patients, confirming their impressive results with conventional colonoscopy and histology. Writing in the November Gastroenterology, Drs. Riccardo Iannaccone, Andrea Laghi, Carlo Catalano, and Roberto Passariello were optimistic that the new technique could result in better screening compliance, and eventually better outcomes population-wide (November 2004, Vol. 127, pp. 1300-1311).
"About one-half of the average-risk population of the United States eligible for screening do not pursue prevention tests.... One of the barriers that may deter participation in CRC (colorectal cancer) screening programs is the aversion of patients to bowel preparation," the authors wrote, citing studies such as the one by Gleucker and colleagues from the Mayo Clinic in Rochester, MN.
Last year the Mayo researchers reported that most patients experience discomfort with cathartic bowel preparation, and that most would be willing to shorten the interval between colorectal screening exams if bowel cleansing were eliminated (Radiology, May 2003, Vol. 227:2, pp. 378-384). Other studies concluded that eliminating cleansing could increase CRC screening compliance.
Iannaccone and colleagues examined 203 patients (141 men, 63 women ages 36-80, mean age 60.5) who were scheduled to undergo CRC with conventional colonoscopy. About half of the patients were asymptomatic (n = 105), including patients with no indications (n = 46), and those with a family history of colorectal cancer (n = 32) or a personal history of polyps (n = 19). Ninety-eight patients were symptomatic, including some with hematochezia (n = 38) or a change in bowel habits (n = 23).
The study examined the patients with multidetector-row CT followed by conventional colonoscopy within three to seven days thereafter. Forty-eight hours before imaging, the patients began drinking 20 mL of an oral iodinated contrast agent (diatrizoate meglumine and diatrizoate sodium 200 mL at 370 mg/mL iodine, Gastrografin, Schering, Berlin) along with five meals a day. Cautioned to avoid fiber-rich foods such as fruit, vegetables, and whole-grain breads and cereals, participants had no other dietary restrictions for the two days preceding the exam.
Following administration of 20 mg of hyoscine-N-butylbromide (Buscopan, Boehringer Ingelheim, Ingelheim, Germany) as an antispasmodic agent (n = 189) or glucagon (n = 14) in those who were contraindicated for Buscopan, the patients underwent manual room air insufflation of the colon to tolerance, in the left lateral decubitus position.
Prone and supine CT images of the abdomen and pelvis were acquired on a Somatom Plus 4 Volume Zoom scanner (Siemens Medical Solutions, Erlangen, Germany) using a 2.5-mm slice thickness, 3.0-mm reconstruction interval, 1.0-mm table speed, 140 kVp, and 10 effective mAs. The group had previously optimized the low-dose protocol.
Data postprocessing was performed using the Vitrea2 software package (Vital Images, Plymouth, MN), and examined separately and independently by three experienced gastrointestinal radiologists who were blinded to the endoscopic results. A segmental unblinding technique was used, by which the gastroenterologist learned of the VC results after each segment was examined in colonoscopy, with the ability to reinsert the colonoscope if the VC results were positive. The group relied on primary 2D interpretation with 3D used as a problem-solving technique.
"This segmental unblinding has been previously adopted to minimize the possibility that false-negatives from optical colonoscopy would be recorded as false-positives on CTC," the authors wrote. All retrieved polyps were examined with histology.
The envelope please
Final unblinded colonoscopy results revealed 162 polyps, including 83 (51.2%) 1-5 mm in diameter, 55 (33.9%) 6-9 mm in diameter, and 24 (14.8%) 10 mm or larger, the group reported. Histology showed that 75/162 polyps (46.3%) were non-neoplastic, while 87 polyps were deemed neoplastic, including 67 tubular adenomas (41.3%), nine tubulovillous adenomas (5.5%), two serrated adenomas (1.2%), three carcinomas in situ (1.8%), and six invasive carcinomas (3.7%).
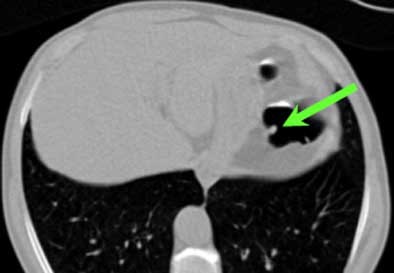 |
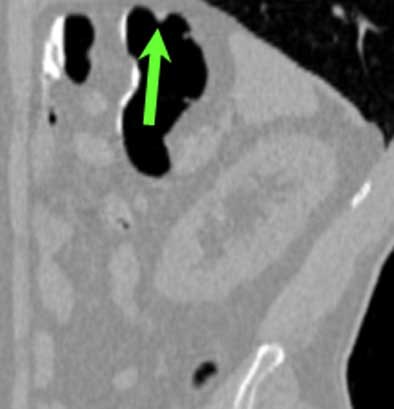
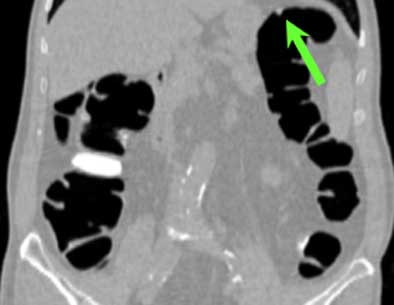
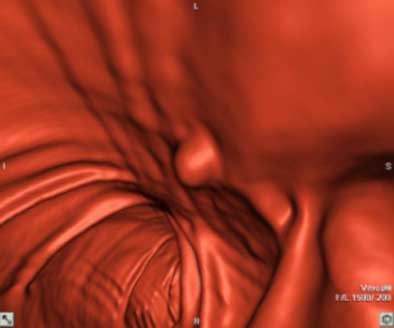
| Top to bottom: A 10-mm polyp in the splenic flexure can be seen in axial, sagittal, coronal, and 3D views. All images courtesy of Dr. Riccardo Iannaccone, University of Rome "La Sapienza." |
 |
 |
 |
Per patient, virtual colonoscopy yielded an average sensitivity of 89.9% (95% CI, 90.9%-96%), average positive predictive value of 88% (95% CI, 83.3%-91.5%), and average negative predictive value of 93.5% (95% CI, 90.9%-96%), the authors wrote. In the more rigorous per-polyp analysis, VC's overall sensitivity was 64.4% (95% CI, 60.2%-68.7%; 72% for neoplastic polyps), including 95.5% sensitivity for polyps ≥ 8 mm (95% CI 92.1%-99%; 100% for neoplastic polyps), and 86% for polyps ≥ 6 mm (95% CI, 81.7%-90.5%).
Virtual colonoscopy produced 16, 16, and 21 false-positives for each of three readers, most due to the presence of thickened folds, and surprisingly in the prep-free study, few false-positives (4, 4, and 5, respectively) were due to fecal material. "This result is correlated to the fact that the use of an effective fecal tagging strategy in our study helped the readers in the differentiation between fecal material and colonic polyps," the authors wrote.
There were also 54, 57, and 52 false-negatives at VC, with no clear cause determined for 59, 51, and 53 of them, even in retrospective analysis. These may have been due to the limits of spatial resolution in the image data, but most of the lesions carried a very low likelihood of malignancy, the group noted. Interobserver agreement between the three readers was high both per-polyp (k = 0.61-0.64) and per patient (k = 0.79-0.91).
Conventional colonoscopy missed five polyps in three patients, all of which were found after segmental unblinding, and all of which were located behind haustral folds. Virtual colonoscopy produced no complications, while one colonoscopy patient was hospitalized for bleeding.
Average negative predictive value of 93.5% was the highlight of the study, the authors noted. "Indeed, as noted by Pineau et al, the negative predictive value of (VC) represents the ability of this examination to correctly identify those patients who do not need to undergo optical colonoscopy," Iannaccone and colleagues wrote (Gastroenterology, August 2003, Vol. 125:2, pp. 304-310). "The clinical impact of this issue can easily be understood, considering that 46%-85% of screening colonoscopies identify no clinically significant pathology."
Better with 2D?
Having relied successfully on primary 2D interpretation with 3D problem-solving, the Italian group credited this approach with faster results in its study discussion, dipping a toe into a controversy that has divided the virtual colonoscopy community. The question is whether 2D primary image interpretation with 3D problem-solving -- or the other way around -- produces the best results overall. Dr. Perry Pickhardt and colleagues championed the 3D primary read as the easiest and most accurate approach in their highly successful study last year (New England Journal of Medicine, December 4, 2003, Vol. 349:23, pp. 2191-2200). But Iannaccone's group took issue with the notion that primary 3D is the only way to fly.
"Notably, in our study, average image interpretation time was 9.8 minutes, which is substantially lower than the reading time reported by Pickhardt et al (average reading time, 19.6 minutes)," the Italian researchers wrote in their study discussion. "The difference can be explained with our primary two-dimensional approach for the analysis of CTC examinations, in which coronal and sagittal multiplanar reconstructions as well as three-dimensional images are used to confirm and better characterize suspected polyps. By contrast, Pickhardt et al based image interpretation primarily on three-dimensional images, which can potentially be more time-consuming. Specific studies are needed to compare a primary two-dimensional with a primary three-dimensional reading to better understand the specific advantages and limitations of each methodology."
Responding in an e-mail to AuntMinnie.com, Dr. Perry Pickhardt noted that his group's reading times "are now in the 5-10 minute range, as the speed of 3D fly-through has doubled and the prep has been refined" since the 2003 Department of Defense study was completed. (Pickhardt and colleagues use software by Viatronix of Stony Brook, NY.)
Pickhardt said the Italian study was carefully conceived and well-performed, representing "an important first step" toward an alternative to cathartic bowel cleansing in some patients. However, he added, the prepless approach is unlikely to provide a singular solution for colorectal cancer screening because it would make same-day conventional colonoscopy impossible. As a result, patients with significant findings on VC would instead have to return home for a complete prep before they could return for conventional colonoscopy and polypectomy. Finally, Pickhardt wrote, the effects of reader fatigue in a 2D reading environment are likely to be significant, and must be accounted for and studied in further validations of the prepless VC.
Limitations
The group's use of iodinated oral contrast (diatrizoate meglumine and diatrizoate sodium) for fecal tagging was both unusual and effective. The iodinated agents, commonly used in the gastrointestinal tract in standard CT exams, meet the criteria for an ideal contrast agent, the authors wrote. They cautioned, however, that the presence of iodine could lead to possible adverse reactions (and did in 10.3% of the patients), including nausea, vomiting, skin reactions, and diarrhea. The very real potential for delayed hypersensitivity reactions did not occur in the present series, they added.
Unlike some studies, this group did not apply digital subtraction to the tagged fecal material before reading the data, largely because the feature wasn't available on their software. Although subtraction can add artifact, it needs to be examined further in future studies, they wrote. Also, the group's use of a fixed dose (200 mL) of tagging agent was considered a limitation because it did not account for differences among patients. Finally, the authors noted, 51.7% of the patients were symptomatic; the relatively polyp-rich cohort could not be considered a true screening population with its associated lower prevalence of lesions.
When asked for their opinions after the studies 24 hours or less after conventional colonoscopy, 79.8% of the patients said they preferred VC with fecal tagging to optical colonoscopy, and 61.1% said they would prefer VC next time. Still, more than a third of patients (35.2%) still said they preferred conventional colonoscopy, perhaps due to its therapeutic capabilities, Iannaccone and colleagues speculated. And asking for opinions so soon after colonoscopy could have skewed the results in favor of VC, they added.
"Our study shows that the performance of low-dose multidetector CTC without cathartic bowel preparation compares favorably with that of optical colonoscopy," they authors concluded. "This examination can be effective in identifying patients without colorectal polyps, thus potentially obviating the need for many unnecessary endoscopic examinations."
By Eric Barnes
AuntMinnie.com staff writer
November 23, 2004
Related Reading
Reduced-prep VC with tagging works after failed colonoscopy, April 7, 2004
New tagging, subtraction techniques aim for better compliance in VC, March 8, 2004
Experience sharpens role of IV contrast-enhanced VC, January 19, 2004
German group optimizes barium-sulfate tagging in MR colonography, January 22, 2003
Fecal tagging improves detection in virtual colonoscopy, August 29, 2002
Prepless virtual colonoscopy shows early promise, June 3, 2002
Copyright © 2003 AuntMinnie.com




















