MDCT can identify coronary plaque type in most patients with suspected coronary artery disease, and even correlate mixed plaque composition with acute coronary syndrome (ACS) presentations, according to a new study from Innsbruck Medical University in Austria.
The results could potentially lead to an expanded role for CT in identifying high-risk patients with vulnerable plaques who require more aggressive treatment and follow-up than those with more stable calcified plaques.
The pilot study, presented at the 2006 European Congress of Radiology in Vienna, sought to determine whether different coronary plaque types as assessed with 16-slice multidetector computed tomography (MDCT) could be correlated with acute coronary syndromes (ACS).
Vulnerable coronary plaques of noncalcified or mixed composition are known culprits in the development of ACS. And CT has demonstrated its ability to distinguish noncalcifying from calcifying plaques.
For example, in a comparative study with intravascular ultrasonography (IVUS), lipid-rich plaque had a mean CT density of 49 HU ± 22 standard deviation (SD), fibrotic plaque had 91 HU ± 22 SD, and calcifying plaque had 391 HU ± 156 SD. "However, the majority of coronary plaques are mixed calcifying/noncalcifying," lead investigator Dr. Gudrun Maria Feuchtner explained in an e-mail to AuntMinnie.com.
"Noncalcifying plaques represent early stages of atherosclerosis, which later develop to vulnerable plaques," she wrote. Vulnerable plaques have an atheroma mass > 40%, a thin cap < 250 µm, a lipid core, central necrosis, signs of inflammation, and microcalcifications leading to plaque instability. Additionally, a positive remodeling index (plaque area exceeding vessel area) has been proposed as an indicator of plaque vulnerability."
For this study, ACS was defined as "chest pain, troponin T elevation, and (non-ST-segment elevation myocardial infarction) ECG alterations," Feuchtner said in her ECR talk. However, it is unknown whether the presence of CT-detected noncalcifying plaques correlate with a risk of acute cardiac events.
Feuchtner, along with Dr. Guy Friedrich, Dr. France Weidinger and colleagues sought to determine whether such a link could be established. The group examined 63 consecutive unselected patients who underwent 16-slice MDCT coronary angiography (Sensation 16, Siemens Medical Solutions, Erlangen, Germany). Images were acquired with the aid of retrospective ECG gating (60%-80% RR interval) using 16 x 0.75-mm collimation, 0.42-sec rotation speed, table speed of 6.7 mm/sec, 120 kVp, and 500 mAs, following administration of 100 mL of Visipaque (iodixanol, GE Healthcare, Chalfont St. Giles, U.K.) at a flow rate of 3-4.5 mL/sec.
Data were reconstructed using a medium smooth convolution kernel and an effective slice thickness of 1 mm with 0.5-mm increments, and were analyzed retrospectively on a workstation.
American Heart Association segment-based classification guidelines were used to analyze only the proximal segments. The observers classified coronary plaques into four types: type 1 calcified, type 2 mixed (composition more calcified than noncalcified), type 3 mixed (more noncalcified than calcified), and type 4 noncalcified. All patients underwent cardiac catheterization, and 17 patients also underwent intracoronary ultrasound, with which the results were correlated, Feuchtner said.
According to the results, 92% of the patients had coronary plaques (type1 31%, type 2 17%, type 3 28%, type 4 24%). The presence of a noncalcifying plaque component (type 2-4 40 of 63; 63%) was correlated with an acute cardiac event (n = 15, 24%; p < 0.001). Mixed plaque type 3 was correlated with an acute cardiac event (p = 0.001), while mixed plaque type 2 and type 4 were not (p = 1 and p = 0.3, respectively).
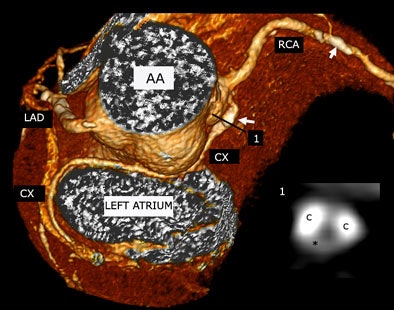 |
| Plaque type 2 (mixed, predominantly calcifying) in a 72-year-old man with stable angina pectoris was found in an aberrant circumflex (CX) arising from right coronary (RCA) ostium and coursing between ascending aorta (AA) and left atrium (LA) distally. The inlay (1) shows a cross-sectional slice of the proximal CX plaque, white arrow is pointing at calcification. A small noncalcifying plaque component (hypodense) was found between two calcifying plaque (C) components. All images courtesy of Dr. Gudrun Maria Feuchtner. |
"The vast majority of patients -- 58 -- had coronary plaques, and not surprisingly, the highest prevalence of purely calcified plaques was found in patients wtih stable angina pectoris" (12 of 18, 66%), Feuchtner said. A Spearman's rank correlation test showed that increasing severity of clinical presentation was associated with increasing noncalcifying plaque component (r = 0.46, p = 0.003).
"Patients with a noncalcified plaque component ... correlated with ACS; however, only mixed plaques correlated with acute coronary syndrome. Exclusively noncalcified plaques were not related to acute coronary syndromes," she said.
"We found that only plaque type 3 was linked to acute coronary events, supporting the concept that vulnerable plaques have a positive remodeling index," Feuchtner stated. "If we look at CT density, a decrease in CT density (corresponded to) a slightly higher noncalcifed plaque component; however, no statistically significant difference was found" and there was significant overlap, she said.
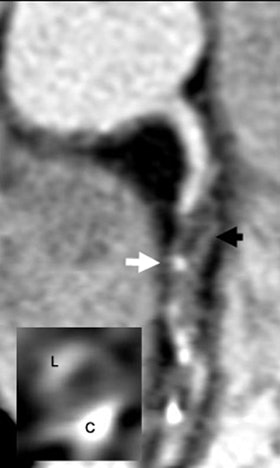 |
| Plaque type 3 (mixed, predominantly noncalcifying) in 64-year-old man in whom non-ST-segment elevation myocardial infarction (NSTEMI)/ACS was recorded 10 days prior to 16-slice MDCT examination. Black arrow denotes hypodense, dark, noncalcifying plaque component. White arrow is pointing at a small calcifying spot. The inlay bottom-left shows a cross-sectional image of the right coronary artery (RCA) at the level of the white arrow. C = calcifying plaque component, L = lumen. Note that hypodense, black noncalcifying plaque is located between C and L. The lesion was graded as 90% stenosis with interventional coronary angiography. |
As measured in 31 patients, the CT density of noncalcifying plaque type 2 was a mean of 94.1 HU ± 44.1 SD, versus a mean of 81.6 HU ± 57.6 SD in noncalcifying plaque type 3, and a mean of 60.3 HU ± 47.7 SD in purely noncalcifying plaque.
Vulnerable plaques may in fact turn out to have lower densities, but the differences are not readily identifiable on 16-slice MDCT, Feuchtner wrote. "Probably the lipid core of vulnerable plaques is too small to be identified based on CT-density measurment (due to) limited spatial resolution."
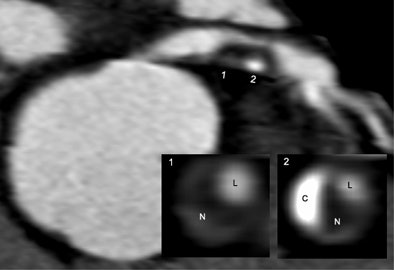 |
| Plaque type 3 (mixed, predominantly noncalcifying) was identified in a 68-year-old man with de novo unstable angina pectoris. Interventional coronary angiography confirmed proximal 90% stenosis of the left anterior descending (LAD) artery. Inlay bottom-right: Images 1 and 2 show cross-sectional images of the plaque. N = noncalcifying plaque component, C = calcifying plaque component, L = lumen. |
The recent addition of a 64-slice CT scanner (Brilliance 64, Siemens Medical Solutions) to Feuchtner's institution is expected to improve plaque imaging due to its higher spatial resolution (0.4 mm3), she added.
In the study, MDCT correctly classified plaque types in 15 of 17 patients compared with IVUS. Forty-five of 63 patients had at least one coronary stenosis greater than 50% at coronary catheterization for a CT sensitivity of 98% (43 of 45), specificity of 90%, and negative and positive predictive values of 97% each.
Of the two out of 17 patients deemed positive for stenosis on MDCT without coronary artery diesase, one had a coronary anomaly and one acute myocarditis.
"In the right coronary artery there is significant stenosis," she said of a CT image of a patient with myocarditis. "On the left lateral wall is acute myocarditis and pericardial effusion not seen on echo."
Noncalcified plaques seen with MDCT can be correlated to ACS, suggesting higher vulnerability for these plaques, Feuchtner said.
"However, only mixed noncalcified plaques correlated to ACS, supporting the concept that positive remodeling is related to noncalcifying plaque," she said. "MDCT may have the potential to identify high-risk patients who may be treated more aggressively if noncalcifying plaques are seen, for example (treatment) with high-dose statins," which have anti-inflammatory effects on plaques and may lead to their regression and stabilization. Frequent follow-up is also needed in patients with noncalcified plaques, she said.
In any case, she said, the results cannot be used to predict the time to occurrence of an acute cardiac event, adding that the group's preliminary results will need to be confirmed in larger prospective studies.
In response to a question from the audience, she said that MDCT won't replace the need for angiography in most cases.
"If you see a stenosis and the lesion must be stented, you have to refer the patient to angiography," Feuchtner said. "But if you can exclude significant stenosis -- for example, if you have myocarditis -- then you could avoid angiography." Using her present study population as an example, only about 10% of the patients could avoid angiography, Feuchtner said.
By Eric Barnes
AuntMinnie.com staff writer
April 20, 2006
Related Reading
Cardiac imaging dazzles, but radiologists can't compete alone, April 10, 2006
Ventricular dysfunction not enough to identify sudden cardiac death risk, March 28, 2006
New cardiovascular CT has high degree of agreement with coronary angiography, February 28, 2006
Multiple reconstructions needed for accurate MDCT calcium scoring, February 14, 2006
MDCT still can't differentiate between noncalcified plaques, January 10, 2006
Copyright © 2006 AuntMinnie.com