SAN FRANCISCO - One of the largest studies to date has also produced some of the highest sensitivities for the detection of ischemic stroke with CT angiography. In the study from the New Jersey Medical School, multidetector CT angiography (MDCTA) was all but equivalent to invasive catheter angiography for the detection of cerebral aneurysms in patients with subarachnoid hemorrhage.
Previous studies have yielded varying sensitivities and specificities for CTA, although its performance has improved in recent years with the increase in the number of detector rows.
The study, presented today at the American Association of Neurological Surgeons (AANS) meeting, found that CTA was statistically equivalent to conventional angiography in patients with subarachnoid hemorrhage, which results from the rupture of an intracranial aneurysm in as many as 85% of patients.
Catheter-based cerebral angiography has been the gold standard for decades, and is highly sensitive thanks to continuing improvements in image quality. But the invasive procedure is not without risk. For example, digital subtraction angiography (DSA) for the examination of subarachnoid hemorrhage has been reported to have a 2.6% rate of rehemorrhage if performed within six hours after the initial event. In addition, the time delay in obtaining the study, operator skill dependence, and high costs are still disadvantages of DSA, said Dr. Charles Prestigiacomo, who presented the results at the meeting.
Another important noninvasive modality, MR angiography, is an excellent screening tool for the detection of unruptured intracranial aneurysms as small as 2-3 mm, but it can also produce significant false positives -- up to 16% in one study. And CTA, though its performance has improved with the advent of multidetector-row CT, still routinely comes up short of angiography.
The study from New Jersey Medical School and University Hospital, both in Newark, was led by Dr. Aria Sabit, along with Prestigiacomo, Pinakin Jethwa, and Jonathan Russin.
DSA retains some important advantages, Prestigiacomo said, "including the high resolution of the 1024 x 1024 matrix, as well as the lack of any venous contamination, and unlimited projections when you use concurrently the 3D subtraction angiography that is now available," he said. "Indeed, 3D subtraction angiography with rotational mode (although not used in the present study) has picked up a total of 47% more aneurysms than conventional DSA has in the past, and has helped with finding the neck and surgical planning of the lesions."
"The advantages of CTA are its noninvasive nature, the rapid imaging, the fact that there may only be a (contrast) reaction as a possible complication, the unlimited projections that can be obtained in 2D and 3D, the fact that you can interrelate the bony anatomy with aneurysms, and the fact that there was, early on, sensitivities ranging from 78% to 96%," he said, adding that the best published studies with MDCT have shown sensitivities as high as 97% compared to DSA. In addition, CTA's radiation dose is still lower than DSA's.
But even 97% sensitivity may not be good enough when facing cerebral hemorrhage. "We cannot afford to miss patients with subarachnoid hemorrhage that have aneurysm, and that has long been a problem with CT angiography," he said.
But considering MDCT's rapid evolution, the group hypothesized that there may no longer be a significant difference between carefully performed CTA and DSA. To find out, they examined patients who were diagnosed with spontaneous subarachnoid hemorrhage based on CT evidence of subarachnoid blood, or positive lumbar puncture when subarachnoid blood was not present.
Over a three-year period that ended in October 2005, CTA was performed on 179 consecutive patients (114 women and 52 men, average age 52.9 ± 13.7 years, range: 14-85 years) with spontaneous subarachnoid hemorrhage, but without neurologic or renal complications.
Images were acquired on a 16-slice LightSpeed scanner (GE Healthcare, Chalfont St. Giles, U.K.) at 120 kVp and 440 mAs (0.625-mm collimation and 0.625-mm reconstruction intervals), following the administration of 150 cc of iodinated contrast injected at a fast 4 cc/sec with an 18-sec scan delay.
Images were reviewed and postprocessing performed on a GE Advanatage workstation, including maximum intensity projections (MIPs) and 3D reconstructions. Data were analyzed by nurosurgical team members trained in CTA. When aneurysms were found, patients were evaluated for possible possible microsurgical clipping or coiling. CTA observations were correlated with angiography.
After CTA, patients scheduled for endovascular intervention underwent four-vessel DSA to confirm the CTA findings and to look for any additional aneurysms. Postoperative angiography was also performed on all patients undergoing microsurgical clipping to assess for residual or additional aneurysms, with intraoperative confirmation of the size and configuration of the aneurysm.
Patients were kept well-hydrated with saline IV hydration to minimize the risk of contrast-induced nephrotoxicity, and those with serum creatinine levels greater than or equal to 1.0 were given oral N-acetylcysteine for eight hours.
Patients with no evidence of aneurysm on CTA underwent a full six-vessel DSA exam, supplemented with 3D rotational angiography (bilateral external carotid arteries, internal carotid arteries, and vertebral arteries) to definitively rule out any anomaly that might have gone undetected at CTA.
According to the results, 166 of 179 patients with spontaneous subarachnoid hemorrhage had at least one intracranial aneurysm detected detected on CTA, for a total of 238 aneurysms. All aneurysms were confirmed either by direct visualization at surgery or by DSA at the time of endovascular treatment, Prestigiacomo said.
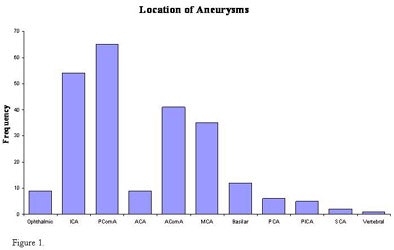 |
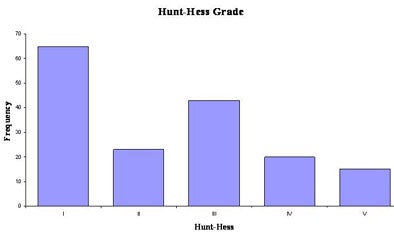
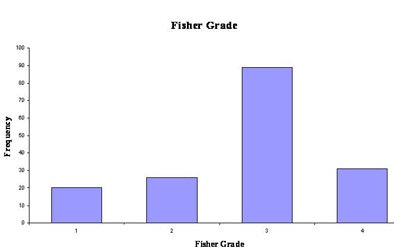
| Figure 1 above denotes the distribution of all aneurysms in the patient cohort. The "ICA" category includes patients who had aneurysms identified in the paraclinoid and paracavernous region, as well as along the course of the supraclinoid carotid artery, but does not include aneurysms of the posterior communicating artery. Detecting aneurysms along bony interfaces and near the cavernous sinus is possible, though difficult. The distributions of Hunt-Hess grade and Fisher grade on admission are presented in figures 2 and 3 (below and bottom), respectively. Charts courtesy of Dr. Charles Prestigiacomo. |
 |
 |
DSA found only one additional aneurysm -- along the distal posterior inferior cerebellar artery (PICA) -- that was not detected prospectively on CTA at the time of presentation. As a result, 238 of 239 (99.6%) aneurysms were initially detected by CTA. Significantly, 88% of the aneurysms detected were subcentimeter, and fully 19% were smaller than 3 mm, he said.
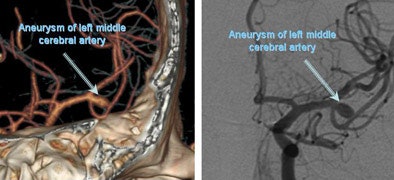 |
| CTA (left) and angiogram (right) shows a single aneurysm of the left middle cerebral artery. Images courtesy of Dr. Charles Prestigiacomo. |
The missed aneurysm was not the one that ruptured, "and was cut off on the 3D reconstruction," Prestigiacomo said. "Retrospective analysis of the source images and reconstructions on 3D once the appropriate cutoffs were made did clearly demonstrate the aneurysm, so this was a postprocessing problem."
CTA's specificity was 100%, as all lesions identified as aneurysms on CTA were confirmed by DSA or direct surgical visualization, and both the positive and negative predictive value of CTA was 100%. The receiver operating characteristic (ROC) curve confirmed an area under the curve of 99%, consistent with the reported sensitivity.
Prestigiacomo credited CTA's high sensitivity to multiple detector-row acquisition, submillimeter sections, and rapid contrast injection of 4 cc/sec.
He cautioned that the high prevalence of aneurysms in the patient population may have led to "expectation bias" that might have nudged the results upward, Prestigiacomo, "and so we looked at (the results) with a very careful eye."
The diminished ability to detect aneurysms near bony interfaces and the cavernous sinus are additional limitations of CTA, he said. Finally, CTA is a nondynamic study, and DSA's dynamic nature can offer important contributions to the nature of a particular aneurysm.
"I think the biggest benefit in our study is the protocol that's used in sorting through the data, and that is that each source image is assessed in a systematic way: right left, internal carotids as well as vertebral arteries ... prior to looking at the MIPs," he said, "and the MIPS are all done at 2-4 mm thicknesses so that you appreciate some of the 3D aspects of the vessels as well as the aneurysms. And only then do you go to 3D reconstructions."
Still to come from the group: Prospective screening studies with 64-slice scanners will assess the limits of resolution in the newest systems, he said, and the results will be compared with the latest MRI protocols as well.
"Will this replace DSA? I think this is one of the steps to get us there," Prestigiacomo said.
By Eric Barnes
AuntMinnie.com staff writer
April 25, 2006
Related Reading
MDCT a good alternative to TTE for aortic stenosis, April 14, 2006
Setting up a cutting-edge 3D lab, April 7, 2006
Stroke etiology detected by transesophageal echocardiography, March 17, 2006
Perfusion CT, MRI agree on most stroke parameters, June 1, 2005
Copyright © 2006 AuntMinnie.com