
By all accounts, imaging has a big future in virtual autopsy, and CT in particular seems headed for a major role. Investigators are finding that noninvasive virtual exams can often do what traditional autopsy cannot, notably in identifying the dead and pinpointing the causes of death.
For most applications, investigators are finding CT to be the fastest and most accurate modality available to carry out this work.
Last year the U.S. Armed Forces Institute of Pathology (AFIP) began using CT as part of its postmortem examination of soldiers. Already the team has performed more than 1,600 exams, acquiring the insight that comes from the careful examination of large numbers of victims who died under tragic circumstances. The researchers' experiences will be detailed in part II of this series.
European radiologists, who pioneered the field of virtual autopsy and taught the U.S. Armed Forces their techniques, cite a number of causes behind the rising demand for noninvasive postmortal exams corresponding to a significant drop in traditional autopsy over the last two decades.
At a time when the cost of traditional autopsies is rising, so are cultural and religious objections that have contributed to a significant decline in many geographic areas.
"In Europe with the decreasing acceptance of autopsy, there's a need for verification of clinical diagnosis. There's a need for clarification in forensic medicine," said Dr. Peter Vock, professor of radiology and chairman of the Institute of Diagnostic Radiology at the University of Bern. Vock introduced a special focus session on postmortem imaging at the 2006 European Congress of Radiology (ECR) in Vienna.
Another advantage of postmortem imaging is the ability to preserve the imaging record long after the body has deteriorated, Vock said. Imaging creates "objective documentation that can be used by any third party," he said. "You can't do that with what you see during a real autopsy. The data are easily distributed, you don't have any motion artifacts, and further you have no limits to radiation exposure."
As for CT, its speed, subtle grayscale, and ability to depict 3D relationships are enormous advantages. Skeletal trauma, for example, can be depicted in ways that conventional autopsy can't replicate.
A close look at the 3D reconstructions can often separate a mortal wound from nonfatal trauma that only looks deadly, which makes the modality indispensable in forensic examinations, Volk said.
Of course, the virtual techniques have inherent drawbacks as well. There is no circulation to image, or other functional information.
"You don't see bleeding," Volk said, adding that blood and bleeding patterns are readily visualized. "You don't see intensity of bleeding. Clots may obstruct the vessels," he said. And in a purely imaging autopsy there is no histology, no chemical analysis, and very tiny findings cannot be followed as they are in conventional biopsy. But "all these disadvantages can potentially be overcome," he said.
Also at the podium during the ECR session was Dr. Michael Thali from the Institute of Forensic Medicine at the University of Bern in Switzerland. He cited several challenges plaguing conventional forensic exams that imaging can potentially overcome.
"Everybody who is working in forensics knows that we have some disadvantages" in conventional autopsy documentation, he said, "especially in the face and pelvic area, where documentation of 3D findings can be subject to different descriptions. It's very important that our visualization is understandable and plausible for the court system."
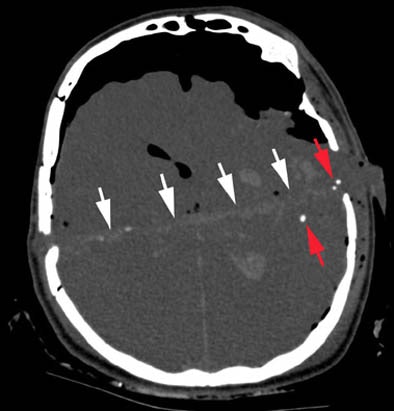 |
| Axial CT scan displaying intracerebral wound track (white arrows) in a case of suicidal gunshot injury. Note the intracranial air and the bullet fragments (red arrows) along the wound track. Image courtesy of Dr. Michael Thali. |
The wrong conclusions surrounding the 1963 assassination of U.S. President John F. Kennedy would certainly have benefited from 3D visualization, Thali said of the infamous autopsy that was plagued (at the very least) by the limitations of poor documentation and 2D photography.
Thus, he suggested, if today's 3D imaging techniques had been available, the "magic bullet theory" (which posits that a single bullet caused all of the nonfatal wounds in both President Kennedy and then Texas Governor John Connally) might have died a very quick death.
Overall, "CT is an excellent tool for the documentation of bone defects and the detection of pathological air or gas in the body, and it's an excellent tool for 2D or 3D reconstruction," Thali said. In cases of mass deaths, dental CT records can be enormously helpful in identifying victims.
 |
| Axial MDCT scan revealing massive air embolism in the heart cavities as well as air in the soft tissues in a fatal diving incident. Image courtesy of Dr. Michael Thali. |
MRI, on the other hand, offers better resolution for organ tissues, and has a "higher evolution potential," than CT, Thali said. In one example of a decomposed body that was found in an apartment two to three weeks after death, MRI was still able to demonstrate a cerebral hemorrhage and indicate the likely cause of death, he said.
In other cases, MR spectroscopy is being used for noninvasively detecting metabolite levels in the brain that change over time, enabling forensic scientists to closely estimate the time of death.
As in living patients, however, CT is always faster than MRI, and can be performed in a few minutes rather than a few hours, he said.
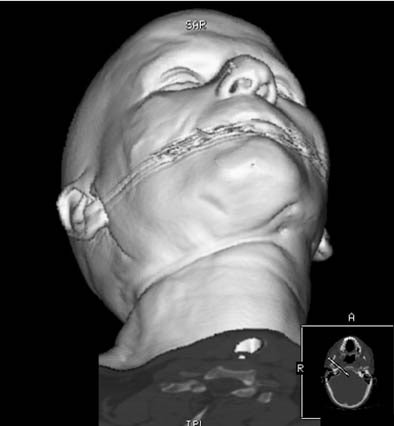 |
| In a suicidal hanging case, 3D CT reconstruction shows strangulation mark around the neck. Image courtesy of Dr. Michael Thali. |
As for the future, "you have to have dreams," Thali said. Forensic pathologists are envisioning an all-in-one virtual autopsy machine that can perform surface scanning and biopsies, as well as high-resolution CT and MRI in about a half an hour. Today's top priorities include the creation of international guidelines for the practice of virtual autopsy, he said.
Postmortem CT
Later in the ECR session, Dr. Anders Persson, director of the Center for Medical Image Science and Visualization (CMIV) in Linköping, Sweden, talked about some of the techniques his center uses for virtual autopsy imaging, particularly in CT.
As the science of postmortem imaging moves from 2D to 3D, "we need to optimize several key parameters, and develop new technologies to carry all the data," he said. "We need to optimize the quality of the dataset. We need small voxel sizes ... and new volume-rendering techniques."
Following the acquisition of a high-quality dataset, the rendering technique is the most important determinant of 3D image quality, Persson said. By depicting the underlying 3D anatomy, good rendering technique can help pinpoint the cause of death.
The highest resolution requires the smallest possible field-of-view, he said. "Always plan to use isotropic volume size, as small as possible." A typical CT acquisition at his facility might examine the inner ear with a small field of view, 0.5-mm collimation, 2-mm thick slices, and 0.1-mm reconstruction interval, Persson said. Applying the same technique to the whole body, even a week after death, creates a highly detailed dataset that can be used to confirm identity or determine the cause of death.
"The drawback is we're getting too many images," Persson said. A normal CT acquisition at the institute these days produces a hard-to-handle 8,000 to 10,000 slices per case. And in a move sure to make matters worse -- and better -- the facility is preparing to install a new dual-source CT scanner this summer.
To deal with the data overload caused by so many high-resolution whole-body scans, the group is using information from the volume-rendering transfer functions at the end of the rendering pipeline -- moving the knowledge it contains to the beginning of the pipeline by rendering only those voxels that contain information, Persson told AuntMinnie.com.
Volume-rendering techniques
"We acquire the images with the smallest possible voxel size, and we have the same resolution with MPRs (multiplanar reconstructions) as with the source images," Persson said.
The group uses minimum intensity projections for gas, and maximum intensity projections for calcifications and foreign body classification, and special volume-rendering techniques that include a new tissue-detection algorithm.
In an e-mail to AuntMinnie.com, Patric Ljung, a Ph.D. student in scientific visualization who creates many of the images at the center, described the group's volume-rendering technique. Before processing, he said, the entire volume (about 1.7 GB of source data in a full-body scan) is divided into small blocks of 16 x 16 x 16 voxels, each of which is stored at multiple resolution levels down to a single average value for all voxels in the block. The process takes about four minutes on a PC. Volume gradients are then computed and a simplified histogram created for each block.
"In run-time we then use these histograms and the current transfer function to determine the visible content of each block," Ljung wrote. Depending on the transfer function visibility, a blockwise level of detail is then determined, and the corresponding resolution levels are downloaded to a graphics card. Blocks with transparent voxels (air, fat, etc.) are assigned a low resolution, while those with large variations are assigned high resolutions.
"Since many voxels in a volume, and consequently blocks, become transparent, we are able to provide high resolution for the remaining blocks using high data reduction," he wrote. "We can go from full-body view to full-resolution closeups in a seamless, interactive fashion."
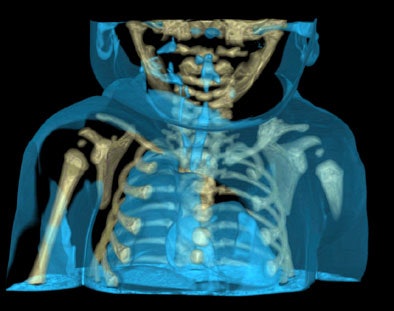
 |
| A traffic accident victim suffered from multiple fractures and died from a broken neck vertebra (below). Images courtesy of Dr. Anders Persson and Patric Ljung. |
 |
Air is completely translucent, and serves as a negative contrast agent in postmortem imaging, Persson said in his presentation.
"We try to preserve the information from the organ into every pixel on the screen," he said. The histograms reflect the voxel values, i.e., Hounsfield units in CT, and intensity values in MR, he said, although MR is more difficult due to the lack of an absolute grayscale. Each voxel is then rated for opacity and brightness.
With the histogram, "you can say these are bone parameters, and you can use it in the next case," Persson said. Both the data and the presets for bone, tissue, etc. can be saved. Using the tissue-classification algorithm, "the computer can find the organs under the surface of the global histogram," and indeed, a number of studies have validated the technique, he said. The technique is reliable, though not foolproof, he said.
Before imaging, workers try to move the body as carefully as possible into the body bag, without moving any body parts. CT images should be acquired as soon as possible after death to minimize postmortem gas. The data are always there in case more investigation or more reconstructions are needed, Persson said.
Virtual autopsy often works where traditional autopsy fails, Persson said, offering an example from his institute, which investigated the case of a 3-week-old infant who had died mysteriously in the operating room during a standard laryngoscopy.
"The autopsy couldn't find the cause of death," he said. But CT showed "a very tiny hole," in the heart, the result of an iatrogenic injury during the procedure.
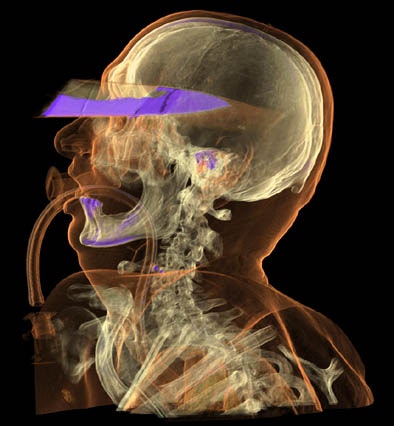
 |
| A 3-week-old infant (above) died mysteriously following laryngoscopy, and traditional autopsy was inconclusive. However, CT showed the cause of death to be a puncture wound to the heart evidenced by an air pocket in the organ (below), which resulted from an iatrogenic injury during the laryngoscopy procedure. Images courtesy of Dr. Anders Persson and Patric Ljung. |
 |
Drowning deaths are another difficult area in traditional autopsy. "But we have a new tool when you use CT -- you can look at lung volume, mean attenuation, anteroposterior differences in attenuation, lung density profile," Persson said.
 |
| In a knife murder case imaged eight to 10 hours after death, CT determined that it was not the head wound that caused the victim's death, but rather a stab wound to the heart, which cut off a carotid artery aorta. Images courtesy of Dr. Anders Persson and Patric Ljung. |
With traditional autopsy it might be possible to approximate the amount of water in the lungs. "But it's much easier to use CT to calculate the voxels and the volume of the lungs," he said. Finally, the CT density profile may differ between drowning and other pathologies, though more research into the precise relationships are needed, Persson said.
By Eric Barnes
AuntMinnie.com staff writers
May 22, 2006
Related Reading
Expanded role envisioned for imaging in autopsies, May 15, 2006
Insight into heart condition tied to athlete deaths, December 21, 2005
Panoramic x-rays prove suitable for dental age calculation, October 12, 2005
CT helps unwrap mummy mystery, May 29, 2005
Radiologic 'autopsy' is already finding evidence without destroying it, December 4, 2003
Copyright © 2006 AuntMinnie.com




















