Sequential transarterial embolization and CT-guided percutaneous cryoablation are feasible and effective for treating renal masses, suggest findings published December 20 in Urologic Oncology: Seminars and Original Investigations.
This approach led to high one- and two-year progression-free survival rates and a low severe adverse event rate, wrote a team led by Matthew Hung, MD, from the Stanford University Medical Center in California.
The researchers said this approach “represents a promising treatment strategy to manage renal masses [greater than or equal to] 3 cm, particularly for those unsuitable for surgery,” Hung and co-authors wrote.
While percutaneous cryoablation can successfully treat small masses or larger lesions in patients not eligible for surgery, its efficacy decreases with larger tumors. This especially goes for renal masses greater than 4 cm in size.
Emerging data suggest that transarterial embolization prior to cryoablation can improve patient outcomes by accurately depicting tumor margins during the latter procedure while decreasing risk of hemorrhage.
Hung and colleagues reported their experience with performing transarterial embolization followed by percutaneous cryoablation for renal masses 3 cm or larger. They focused on therapeutic efficacy and patient safety for their study.
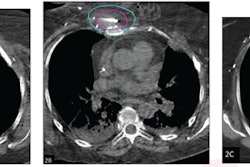
Final analysis included 46 patients with renal masses 3 cm or larger, with 31 patients having masses larger than 4 cm. The researchers reported a median tumor diameter of 4.5 cm. The patients underwent sequential transarterial embolization and CT-guided percutaneous cryoablation between 2014 and 2024 at two institutions.
The team defined primary efficacy as the percentage of target tumors with no evidence of residual enhancement following the initial procedure. Secondary efficacy included tumors that underwent successful repeat ablation after finding local tumor progression. Finally, the team classified adverse events according to criteria set by the Society of Interventional Radiology.
The researchers found the following:
Primary and secondary efficacy rates for T1a lesions (4 cm across or smaller) were 93% and 100%, respectively.
Primary and secondary efficacy rates for T1b lesions (4 cm to 7 cm across) were 81% and 87%, respectively.
One- and two-year progression-free survival rates were 94% and 87%, respectively, after a median imaging follow-up period of 1.6 years.
The approach led to a low overall adverse event rate of 13% and a low severe adverse event rate of 4%.
Both severe adverse events were related to post-procedural hemorrhage, the researchers noted.
The study authors called for future prospective multi-armed studies to establish the efficacy and safety of this approach compared to ablation alone and other surgical and nonsurgical alternatives.
“In comparison to prior studies, our study demonstrates comparable results with the largest patient cohort of sequential transarterial embolization and percutaneous cryoablation reported to date,” they wrote.
Read the full study here.