Percutaneous cryoablation is safe and effective for patients with recurrent or metastatic soft-tissue sarcoma after earlier treatments, suggest findings published July 31 in the American Journal of Roentgenology.
Researchers led by Rahul Sheth, MD, from the MD Anderson Cancer Center in Houston, TX, found high overall survival rates at one and two years after cryoablation, as well as few complications.
“Percutaneous cryoablation should be considered for local control of treatment-refractory soft-tissue sarcoma,” Sheth and co-authors wrote.
Treatment options are limited in patients with recurrent or metastatic disease after initial treatment of soft tissue sarcoma via surgical resection, radiation, or systemic therapy. The researchers highlighted that percutaneous cryoablation could be a complementary, minimally invasive option for these patients.
Sheth and colleagues studied the safety and efficacy of local percutaneous cryoablation performed for treatment-refractory recurrent or metastatic soft-tissue sarcoma.
The study included data collected between 2016 and 2023 from 141 patients with a median age of 66. In total, the patients underwent 217 cryoablation procedures to treat 250 recurrent or metastatic soft-tissue sarcoma lesions, either by CT or MRI guidance.
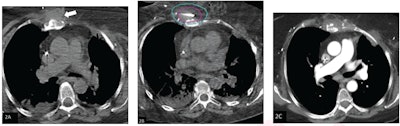 (A) Axial noncontrast CT chest image shows soft tissue mass in the anterior chest wall (arrow). The lesion was treated by percutaneous cryoablation. (B) Intraprocedural axial CT image obtained during cryoablation. The pink outline represents the target lesion and the blue outline represents ice ball. Based on review, the procedure was classified as achieving adequate ablation. (C) Axial contrast-enhanced CT chest image, obtained three months after ablation (patient’s first follow-up exam), shows involution of the target lesion without evidence of residue. Image courtesy of the ARRS.
(A) Axial noncontrast CT chest image shows soft tissue mass in the anterior chest wall (arrow). The lesion was treated by percutaneous cryoablation. (B) Intraprocedural axial CT image obtained during cryoablation. The pink outline represents the target lesion and the blue outline represents ice ball. Based on review, the procedure was classified as achieving adequate ablation. (C) Axial contrast-enhanced CT chest image, obtained three months after ablation (patient’s first follow-up exam), shows involution of the target lesion without evidence of residue. Image courtesy of the ARRS.
For each treated lesion, a single interventional radiologist re-reviewed intraprocedural images to assess for adequate coverage by the ice ball generated from cryoablation procedures. This included coverage of the entire lesion and a ≥ 5-mm margin in all dimensions. The researchers also extracted data on complications and outcomes from medical records.
The most common histologic types found were leiomyosarcoma (n = 56) and liposarcoma (n = 39). The lesions had an average long-axis diameter of 2 cm.
Results included the following:
- Adequate ice-ball coverage was achieved for 82% of lesions.
- The complication rate was 2% (n = 4). This included three major complications and one minor complication.
- The median postablation follow-up was 25 months, including a range of three to 80 months.
- Local progression-free survival was 86% at one year and 79% at two years. Chemotherapy-free survival meanwhile was 45% at one year and 31% at two years.
- Overall survival was 89% at one year and 80% at two years.
Using Kaplan-Meier analysis, the researchers determined that leiomyosarcoma, in comparison with liposarcoma, had significantly higher local progression-free survival. However, there was no significant difference between the two in terms of overall survival.
Finally, in multivariable analysis, the team identified the following factors independently associated with an increased risk for local progression: inadequate ice-ball coverage (hazard ratio [HR] = 7.73) lesion location of the peritoneum (HR = 3.63), and lesion location of the retroperitoneum (HR = 3.71) relative to the lung.
The study authors noted several advantages of cryoablation in this area. These include allowing patients to experience chemotherapy “holidays,” treating multiple lesions in a single procedure, not needing prolonged cessation of systemic therapies, not preventing additional local treatments from happening, and repeatability.
The full results can be found here.