ORLANDO – Sonoporation is a promising method for treating pancreatic cancer, but it has a long way to go, suggest findings presented March 30 at the 2025 American Institute of Ultrasound in Medicine (AIUM) annual conference.
In his presentation, Flemming Forsberg, PhD, from Thomas Jefferson University in Philadelphia, PA, shared his team’s findings from an ongoing phase II clinical trial combining chemotherapy with sonoporation, a therapeutic technique that uses contrast-enhanced ultrasound (CEUS) during chemotherapy concentration in the blood. The idea is that the use of contrast microbubbles changes the vascular microenvironment of a tumor, allowing more chemotherapy to penetrate the tumor.
The team found that this method, so far, leads to changes in CA19-9 blood test levels and increased overall survival for patients under certain chemotherapy regimens, though these findings did not achieve statistical significance.
“These numbers could change and I’m not making any guarantees, but it is at least interesting that we have some encouraging results,” Forsberg said.
Pancreatic cancer is the fourth-leading cause of cancer-related deaths in the U.S., owing to low survival rates. This is due to about half of patients presenting with metastases.
Forsberg said innovative strategies for drug delivery and treatment monitoring are needed to improve patient outcomes. He and his colleagues are leading a phase II clinical trial, where sonoporation is being used to treat pancreatic cancer along with chemotherapy. The team is using the Sonazoid contrast agent (GE HealthCare).
 Flemming Forsberg, PhD, discusses initial results of a phase II study examining the utility of sonoporation in treating pancreatic cancer.
Flemming Forsberg, PhD, discusses initial results of a phase II study examining the utility of sonoporation in treating pancreatic cancer.
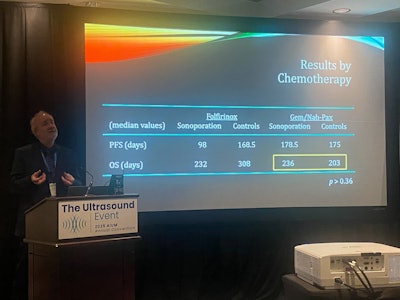
While the trial’s goal is to enroll 120 patients, Forsberg presented data from 65 patients who have complete data available as of March 20. The researchers compared the results to those of patients receiving the standard of care. The team also placed patients into different groups of chemotherapy regimens. Folfirinox was used in 49 patients, of which 25 were in the sonoporation arm. And either nab-paclitaxel or gemcitabine was used for 16 patients, even split into sonoporation and standard-of-care arms.
While sonoporation did not lead to significant improvements for the most part, it did change CA19-9 levels (a protein in which high levels indicate cancer).
| Comparison between sonoporation, standard of care treatment for pancreatic cancer | ||
|---|---|---|
| Measure | Standard of care | Sonoporation |
| Number of chemoTx cycles | 7.5 | 6 |
| Study duration | 104.5 days | 130 days |
| Progression-free survival | 171.5 days | 132 days |
| Overall survival | 281 days | 232 days |
| CA19-9 levels | -36 U/ml | -55.75 U/ml |
Sonoporation also did not lead to significant improvements by tumor staging for cancers at stages II, III, and IV (p > 0.68). By chemotherapy though, patients in the sonoporation arm who were administered nab-paclitaxel or gemcitabine had a median of 236 days of overall survival compared to 203 days for the control group. However, this did not achieve statistical significance (p > 0.36).
While the team reported no adverse events related to Sonazoid administration, 59 serious adverse events occurred in the study, grade 3 or higher. These included 27 events in the sonoporation group compared to 32 in the standard of care group. Also included in the latter group were two grade 4 events and two grade 5 events.
Despite the lack of statistically significant data, Forsberg said the results show that sonoporation could improve the standard of care by increasing pancreatic tumor response to chemotherapy. He highlighted that the more critically ill patients are given nab-paclitaxel or gemcitabine rather than folfirinox.
“It’s also nice to see that we have absolutely no adverse events related to the administration of bubbles, because that’s already something that makes oncologists nervous,” he said.
The researchers are continuing to identify potential candidates for study enrollment.