Percutaneous microwave ablation can be a safe and effective treatment for lung tumors close to the heart and aorta, according to a recent study.
The finding is from a retrospective analysis of outcomes among 40 patients who underwent the minimally invasive procedure between 2017 and 2024, with the authors describing how they achieved technical success.
“Patients should not be excluded from ablation therapy by the location of tumor per se,” noted Yan-Lin Li, MD, of Oxford University Hospitals in the U.K., and colleagues. The study was published January 31 in Clinical Radiology
Microwave ablation is an image-guided procedure that uses electromagnetic waves to heat and kill small cancerous tumors. It is performed percutaneously with a small microwave probe that is guided inside tumors.
Microwave ablation is an option for patients who have a contraindication to surgical resection, such as those with impaired lung function, yet it is not typically performed in patients with lesions close to the heart and aorta due to the risk of inadvertent damage to surrounding tissue, the authors explained. Nonetheless, data on the safety and efficacy of using microwave ablation for these high-risk lesions remains limited, they added.
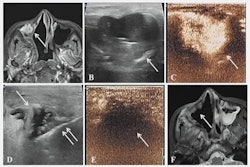
To bridge the gap, the group analyzed outcomes in 40 patients with 44 lung tumors at a median distance of 3 mm from the heart and or aorta who underwent microwave ablation. The median tumor size among patients was 14 mm. Efficacy outcomes included technical success, ablation success, and oncological success, while safety outcomes included clinical success and complications.
According to the results, the technical success rate was 100% and ablation success was 95.4%. There was no inadvertent puncture of the heart or aorta during needle placement nor needle dislodgement by pulsation during the ablation cycles, the researchers reported. Local recurrence was seen at five out of 44 tumor sites during the 12-month follow-up period, making the one-year oncological success rate 87.1%.
Two patients (5%) suffered from severe complications. These were one case of systemic air embolism leading to death and one case of first-degree heart block three months after the procedure.
“We did not observe convincing evidence of damage to the heart or aorta in our cohort. In the only procedure-related mortality, the clinical circumstances were not consistent with aortic rupture,” the authors wrote.
The researchers noted limitations, namely the lack of standardized pre- or postprocedural cardiac assessment for these patients, such as cardiac MRI or echocardiogram, so that they were unable to assess subclinical deterioration. Also, the experience at their center may not be generalizable to other centers, they noted.
“Multicentric registry or prospective studies would be needed to increase the external validity of our approach,” the group concluded.
The full study is available here.