
Among the nearly 30,000 cases of pancreatic cancer diagnosed each year in the U.S., an estimated 5% to 30% have tumors that are contained entirely within the head of the pancreas.
This relatively fortunate subgroup has a better chance of surviving long term via the Whipple, a complex and potentially curative surgical procedure that comes with a rather high complication rate.
Radiologists at Beth Isreal Deaconess Medical Center in Boston are hoping to boost the odds of surgical success with the virtual Whipple, a CT-based planning tool they've developed to give surgeons an idea of what they're going to find step-by-step during the Whipple procedure.
In a presentation at the Stanford University's 2007 International Symposium on Multidetector-row CT in San Francisco, Beth Israel radiologist Dr. Darren Brennan described the color-coded virtual procedure that surgeons at his facility have come to rely on.
Determining which pancreatic tumors are potentially resectable -- or more accurately, which tumors are not -- has long been the province of contrast-enhanced multidetector-row CT, which can depict pancreatic cancers in the context of regional vasculature, eliminating candidates with obvious vascular involvement.
Imaging the pancreas
"When we do pancreatic CTA we do just two phases, a pancreatic parenchymal phase and a portal-venous phase similar to what's been described by other authors," Brennan said in his presentation. "We review the images -- axial coupled with the judicious use of MPRs and MIPs and volume-rendered images."
During the noncontrast and peak arterial phases, there is no differentiation of the pancreatic parenchyma and adenocarcinoma. But the pancreatic parenchymal phase, which follows the peak arterial phase by about 10-15 seconds, shows good differentiation between the two, while the portal-venous phase about 45 seconds later offers the best depiction of the liver, "and a good second look at the pancreatic adenocarcinoma," Brennan noted.
The Whipple treats tumors at the head of the pancreas by removing the pancreas and duodenum, which share the same blood supply, as well as the gallbladder and distal part of the stomach. Newer versions of the Whipple procedure spare the pylorus and proximal duodenum, extending the planning requirements, but potentially offering patients a higher quality of life post-surgery.
The procedure is worth perfecting. Whipple surgery combined with postoperative adjuvant therapy appears to improve median survival in patients with pancreatic adenocarcinomas. Although mortality associated with the procedure for the treatment of pancreatic cancer is less than 2%, complications have occurred in as many as 30%-40% of all Whipple procedures.
Brennan said there is no proof of better outcomes resulting from the virtual Whipple at this stage of research. "We like it -- I don't know how much it's beneficial to the surgeons, but it's obviously very useful," he told AuntMinnie.com.
The most convincing reason for extended preprocedural planning is the considerable anatomic variability in the arterial supply to the region. By preoperatively simulating the surgery on a workstation, the virtual Whipple can help surgeons work around deviant anatomy.
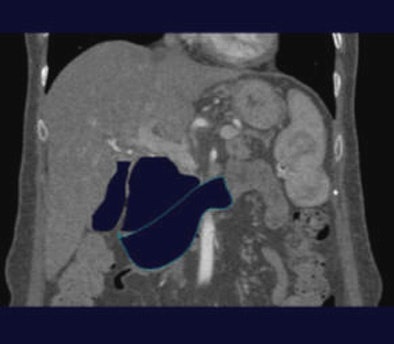
The virtual Whipple begins by manually tracing along the borders of the gallbladder, pancreas and duodenum (images below) using multiplanar reformats to avoid essential anatomy before executing a simple remove algorithm. Subsequently a 3D angiogram can be generated in which arteries which cross through the anticipated surgical planes are color-coded, and thus highlighted to the surgeon.
Brennan's group acquires images on a 64-detector-row Aquilion scanner (Toshiba America Medical Systems, Tustin, CA) following power injection of 20 mL of iodinated contrast (350 mg I/mL) at approximately 5 mL/s. Sequences include an unenhanced late arterial-pancreatic parenchymal phase and early portal-venous phase 20 seconds later, all timed with bolus tracking.
A recent study outlined the typical Whipple procedure, performed in six essential maneuvers, wrote Brennan and colleagues Dr. Giulia Zamboni, Dr. Jacob Sosna, and Dr. Mark Callery et al from Beth Israel in the American Journal of Roentgenology (May 2007, Vol. 188:5, W451-W455).
- The study examined 49 patients with preoperative MDCT scans
- 19/49 (39%) had arterial variants relevant to the Whipple procedure
- Increased mean blood loss in the group with arterial variants versus the group without arterial variants (511 ml versus 376ml)
- 9 patients with replaced right hepatic arteries (RHA)
- 2 Inferior posterior descending arteries (PDA) off replaced RHA
- 3 accessory RHA
- 8 inferior PDA arising from jejunal artery
- 1 posterior superior PDA off celiac artery
- 3 other variants
For planning via the virtual Whipple, arterial-phase MDCT images are sent to an offline workstation (Vitrea 2, Vital Images, Minnetonka, MN). After the algorithm identifies and manually traces the margins of the gallbladder, the organ is isolated and electronically removed from the dataset. Next, the dissection margins of the duodenum and pancreas are drawn, with care to avoid the surrounding vascular structures.
"At the moment these are performed at a 3D workstation by trained 3D CT technologists, though we just recently acquired thin-client sections and we suspect that we (radiologists) are going to be doing these ourselves on the fly," Brennan explained.
 |
| The margins of the gallbladder, here outlined by positive oral contrast post ERCP, are manually traced. All images courtesy of Dr. Darren Brennan. |
The radiologist also creates VR images for each case. "They're much beloved by the surgeons because it enables them to spatially recognize the relationships between crucial vascular structures and the tumor prior to going in and performing the Whipple operation, and they're useful for us as radiologists because they show us the relationship of the tumor to the vessels, to look for relevant vascular anomalies and variants, and also to look for the effect of the tumor on the vessels," Brennan said.
 |
| The gallbladder is then removed by executing a simple remove algorithm. |
The reconstructed images help determine if the cancer is operable, Brennan said.
"We look at the relationship of the tumor to the vessels, and based on the degree of circumferential contiguity between the tumor and the individual arteries and vessels, we can make a determination of likely resectability," Brennan said.
 |
| Above, the removal procedure is then repeated for the pancreas and duodenum using MPRs (below) to avoid accidentally removing critical structures. |
 |
The real Whipple
The actual Whipple operation begins with dissection to the lesser sac and wide exposure of the pancreatic bed, the AJR authors explained.
"Kocherization is used to physically lift the pancreas and duodenum out of the lesser sac to enable further dissection. The next step involves division of the common hepatic duct and performance of cholecystectomy," they wrote. Blunt dissection is performed along the superior mesenteric vein before transection of the pancreatic head, and the head of the pancreas is removed. In a classic Whipple procedure, antrectomy is performed, and the pylorus and duodenum are removed. In a pylorus-preserving Whipple procedure, the pylorus and proximal duodenum are retained. The uncinate process is carefully dissected away from the superior mesenteric vein and removed."
The final step requires mobilization of a loop of jejunum and construction of a pancreati-cojejunostomy, a choledochojejunostomy, and a duodenojejunostomy. The pylorus-sparing procedure is now standard at the institution, the authors wrote.
Anatomic variants to watch out for
For surgical planning it's important to remember that not all pancreatic tumors enhance at MDCTA. Tumors that are iso-attenuating at all contrast phases occur in about 10% of cases, Brennan said. For this reason it is crucial to look for secondary signs of tumor involvement such as dilatation of the vascular cutoff, in order to avoid missing the lesion.
"Always look for metastases, particularly peritoneal, he said. "Mets are probably the Achilles' heel of imaging pancreatic adenocarcinoma."
Even if the tumor is nonenhancing, other CT signs can point the way. The teardrop superior mesenteric vein is a particularly useful sign, demonstrating flattening of the vein touched by a tumor. It is considered an indicator of vascular involvement, "and we have found that it is a relatively good sign in the sense of a predictor of nonresectability," he said.
Also of note, during surgical reconstruction the surgeon needs a good, healthy arterial supply in order to perform a viable anastomosis, such as a pancreatic jejeunostomy, Brennan said. "Therefore, when you review the images preoperatively you should look to see if there is significant arteriosclerosis, or atherosclerosis, or anything that could adversely affect your ability to perform a healthy anastomosis," he said.
Remember that the gastroduodenal artery serves as the conduit between the celiac axis and the superior mesenteric artery, he said.
"In cases of celiac axis occlusion, the branches of the celiac axis, meaning the splenic artery and the common celiac artery, are going to be supplied retrogradely" via the gastroduodenal artery, he explained. "This is important because in the Whipple operation the gastroduodenal artery is routinely sacrificed. If we do not make the surgeon aware of this preoperatively, and he doesn't realize that there's an occluded celiac axis inflow, it can lead to catastrophic problems."
Another variant is the accessory or replaced right hepatic artery, which runs ectopically posterior to the portal vein. "The reason why this is important is because the location can be confused with the cystic artery to the unaware surgeon -- with disastrous consequences," Brennan said.
Describing the venous anatomy preoperatively is also helpful for the surgeon, Brennan said.
"Typically the splenic vein and the superior mesenteric vein will unite to form the portal vein. But the inferior mesenteric vein, having a variable insertion, inserts into the splenic vein in this case," Brennan said of an example.
The jejunal branch usually attaches to the superior mesenteric vein at around the 3 o'clock position, but on rare occasions it inserts ectopically into the superior aspect of the SMV. Why does this matter?
"One of the last things the surgeon does when he's doing a Whipple operation -- and this happens after he's committed to the Whipple operation and there's no going back -- is that he bluntly dissects along the posterior aspect of superior mesenteric vein in order to lift it out and free it from the retroperitoneum," Brennan said. "If there are any ectopically inserting veins that insert posteriorly, particularly the first jejunal branch because it's such a large vessel, it can lead to venous oozing." Again, the surgeon should be made aware, Brennan said.
Doing the virtual Whipple
During the real Whipple procedure, cholecystectomy is one of the first steps performed, Brennan said. "We mimic this electronically (in the virtual Whipple) by manually tracing the margins of the gallbladder. We then follow faithfully the various steps of the Whipple operation, sequentially removing on the workstation the pancreatic head and neck, the duodenum, and finally identifying the uncinate process and removing this -- referring at all times to multiplanar reformatted images so that we don't inadvertently remove vascular structures or important structures."
 |
| Color-encoded angiogram shows an aberrant origin of the right hepatic artery from the superior mesenteric artery (small arrows). As this does not cross through the surgical plane, it is not encoded although documenting its presence preoperatively is important. There is an aberrant origin of a superior pancraticoduodenal artery from this right hepatic artery (large arrow) that is predicted to traverse the surgical plane and which is subsequently color-encoded. |
The radiologist generates VR maps which are color-coded. All vessels that cross through the anticipated surgical field are color-coded in red. The finding that 40% of patients have a relevant variant, and that those with a variant had increased blood loss are key, he said.
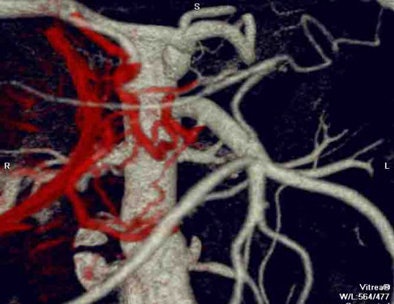 |
| There are multiple complete and incomplete pancreaticoduodenal arcades traversing the surgical plane which are fed from the celiac axis and from various jejunal branches from the SMA. These arteries are color-encoded in red. This patient's operation was complicated by delayed bleeding requiring re-exploration. |
"MDCT allows for comprehensive preoperative assessment of pancreatic adenocarcinoma," Brennan said. "Judicious rendering of the images can aid in identifying the risks going into the procedure."
AuntMinnie.com staff writer
August 16, 2007
Related Reading
High contrast flow rate best for pancreas CT, November 8, 2006
Elderly need less contrast for pancreatobiliary imaging, August 2, 2006
CT features diagnose autoimmune pancreatitis, February 2, 2006
Whipple procedure linked to liver abscesses in hepatic chemoembolization, March 5, 2001
Copyright © 2007 AuntMinnie.com




















