Radiologists routinely administer both an oral barium suspension and IV contrast for evaluating suspected appendicitis, diverticulitis, and small-bowel obstruction (SBO). Would studies work as well without oral contrast? And what about oral iodine? Can it replace barium in abdominal applications other than virtual colonoscopy, in which it is gaining favor?
At the 2007 RSNA meeting in Chicago, two research groups explored these issues in back-to-back presentations. First, radiologists from the Boston University Medical Center (BUMC) compared CT's ability to diagnose two groups of patients with abdominal pain: one scanned with oral and IV contrast, and the other with IV contrast alone.
Next, a team from the University of Texas in Dallas recounted "a tale of two viscosities," comparing CT results in two groups of adult emergency department patients referred for abdominal/pelvic CT. One group received barium, and the other iohexol, a nonionic iodinated oral contrast agent.
Both studies found good results without barium. But both relied on separate patient groups for each protocol, meaning that larger cohorts will be needed to confirm the findings.
Dropping oral contrast
"We recently did a study evaluating patients with nontraumatic abdominal pain without the use of oral contrast," said BUMC's Dr. Stephan Anderson in his presentation.
Anderson's cohort included 303 adult patients (140 men, mean age 43 years) with nontraumatic bowel pain, suspected of having one of three common diagnoses. All patients received IV contrast and were randomized to receive oral barium sulfate versus no oral contrast, Anderson said. The co-investigators included Dr. Jorge Soto and Dr. Brian Lucey.
"The purpose of our study was to prospectively compare IV-contrast-enhanced 64-slice MDCT images obtained with versus without oral contrast for the diagnosis of appendicitis, diverticulitis, or small-bowel obstruction," Anderson said.
Between April 2006 and January 2007, 150 patients were randomized to receive IV contrast only, and 152 received IV contrast plus an oral barium sulfate suspension. One indeterminate study was eliminated from analysis.
All images were acquired using a LightSpeed VCT scanner (GE Healthcare, Chalfont St. Giles, U.K.) using 1.25-mm slice thickness and a noise factor of 19, Anderson said.
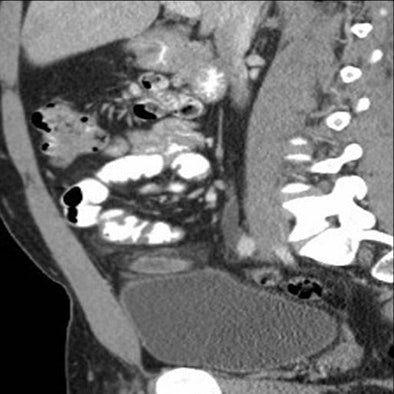
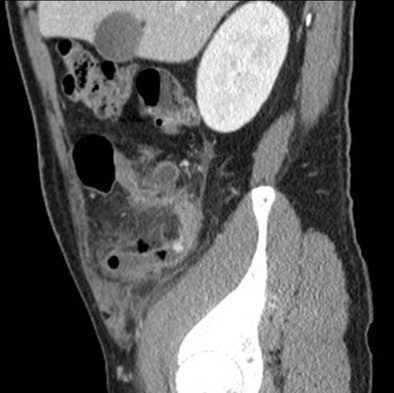
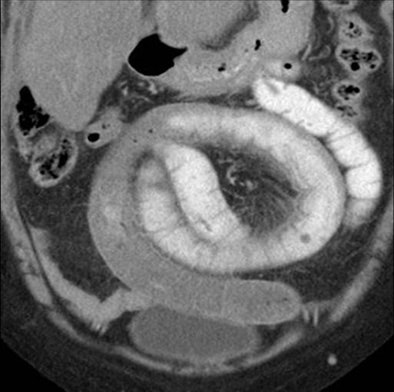 |
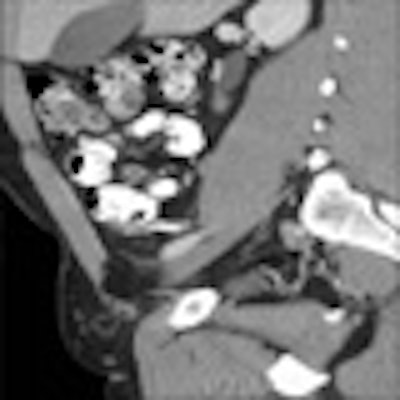
| Above, small-bowel obstruction diagnosed with both oral and IV contrast. Below, another patient with small-bowel obstruction diagnosed with IV contrast alone. All images courtesy of Dr. Stephan Anderson. |
 |
"We routinely inject 100 mL of IV contrast and image at 70 seconds (scan) delay for our portal venous phase," he said. "For our oral contrast arm, our patients received 900 mL of positive oral contrast material, and they underwent a controlled two-hour preparatory time before the CT scan was acquired."
Each scan was reviewed by at least two of three expert emergency department radiologists, who independently evaluated the images for appendicitis, diverticulitis, and small-bowel obstruction using a five-point scale. In case of disagreement between two radiologists, the third radiologist was asked to break the tie. The readers examined "axial, MPR (multiplanar reconstruction), and postprocessing options as they saw fit," Anderson said.
Clinical outcomes, including pathology reports, were used as the reference standard. The study was powered at 90% to detect a 10% difference in either sensitivity or specificity, Anderson said.
Among the 150 patients receiving both oral and IV contrast, 14 had appendicitis, 12 had diverticulitis, and three had small-bowel obstructions. Among the 152 patients receiving IV contrast alone, 14 had appendicitis, 11 had diverticulitis, and seven had small-bowel obstructions.
 |
| Above, small-bowel obstruction diagnosed with both oral and IV contrast. Below, another patient with small-bowel obstruction diagnosed with IV contrast alone. |
 |
For diagnosing one of the three conditions, CT with IV contrast alone had a sensitivity of 87.1% (95% CI, 70.2% to 96.4%) and specificity of 92.6% (95% CI, 86.4% to 96.5%). CT using both oral and IV contrast showed a sensitivity of 82.8% (95% CI, 64.2% to 94.2%), and specificity 95.9% (95% CI, 90.6% to 98.6%).
Surgical confirmation was available for the appendicitis cases. "In the oral and IV group, 14 patients had surgically proven appendicitis; sensitivity and specificity for the CT scans being 100% and 98.5%, respectively," Anderson said. "For the IV-only group, 13 patients had surgical proof of appendicitis; sensitivity and specificity being 100% and 98.5%, respectively, as well."
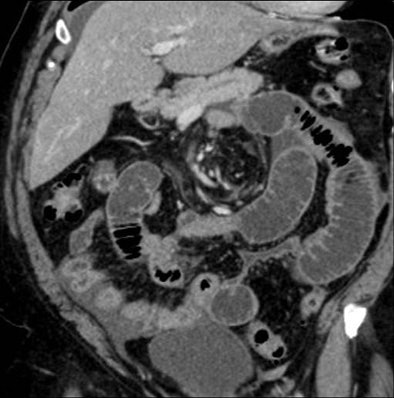
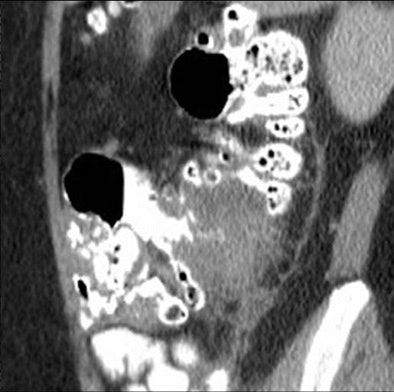
 |
| Above, appendicitis diagnosed with both oral and IV contrast. Below, another patient with appendicitis diagnosed with IV contrast alone, both with surgical confirmation. |
 |
For the clinical diagnosis of diverticulitis, CT yielded a sensitivity and specificity of 91% and 99%, respectively, in the oral and IV contrast group (11 patients), and sensitivity and specificity of 90% and 97%, respectively, in the group that received only IV contrast (10 patients).
The researchers found a trend toward better results using IV contrast alone, but lacking a sensitivity difference of at least 10% between the two approaches, the study was not statistically powered to declare a winner.
However, it was possible to conclude that 64-slice CT with IV contrast alone achieved performance similar to combined IV and oral contrast for the diagnosis of appendicitis, diverticulitis, and small-bowel obstruction together, Anderson said.
"Given the power of the study and low frequency of abnormal scans, we are unable to make conclusions about individual diagnoses," Anderson said.
And eliminating oral contrast speeds up patient throughput by eliminating the two-hour prep period, he added. But for now, the group is still administering oral contrast along with IV contrast.
After the talk, session moderator Dr. William Mayo-Smith, a professor of radiology at Brown University in Providence, RI, said that IV contrast alone seemed just as promising in his institution, where emergency department physicians evaluate about 100 patients a day presenting with intra-abdominal pain.
"We're getting a lot of pressure from our ER physicians and the hospital to increase throughput in the ER and decrease turnaround time," Mayo-Smith said. "About a year and a half ago, we stopped using oral contrast with expectations of calling patients back, but that really hasn't happened.... So our findings clinically and anecdotally reflect this study, which is that you don't need to use it. Sometimes it's actually nicer not to have oral contrast because you can see mucosal enhancement of the appendix better than you see with oral contrast."
In response to a question from the audience, Anderson said that judging the transit time of oral contrast may be helpful in diagnosing small-bowel obstruction.
A tale of two viscosities
In the second RSNA presentation, Dr. Lea Alhilali and colleagues from the University of Texas at Dallas aimed to compare the use of 2% barium sulfate solution to iohexol, an iodinated nonionic monomer agent given orally to patients presenting to the emergency department with abdominal pain.
"Emergency radiology shoulders the difficult task of trying to balance the clinical need for rapid diagnosis with a radiology obligation to maintain image quality," Alhilali said. "Among the exams performed in the emergency setting, exams of the abdomen are among the most time-consuming because of the time delay necessary to allow adequate passage of oral contrast.... Iodinated agents present an interesting alternative to barium because they have a lower density and lower viscosity, which in theory allows for more rapid bowel transit.
The iodinated agents also have a direct stimulatory effect on peristalsis, which enhances peristalsis and thus bowel transit, she noted. Still, theories of iodine's superiority to barium have not held up in clinical studies, which have found iodinated agents inferior to barium both in transit times and opacification -- "and patients actually prefer barium," Alhilali said.
The chasm between theory and clinical results is due in part to an additive to high-osmolality agents to decrease their toxicity, which also increases viscosity and transit times. Low-osmolality agents on the other hand do not have an additive, and studies have shown adequate transit times when polyethylene glycol is added to the mix, she said.
Alhilali and her colleagues Michael Seymour, Dr. Jeffrey Pruitt, and Dr. Julie Champine sought to determine whether dilute iohexol could be an effective oral contrast alternative to barium for abdominal pain patients in the emergency setting, where time is of the essence.
The two protocols were compared in two patient groups. Fifty-nine patients in group 1 were given 900 mL of a 2% barium sulfate suspension with water in three doses (450 mL one hour before scanning, 225 mL 30 minutes before scanning, and 225 mL immediately prior to the study). Group 2, consisting of 169 adult emergency department patients received 465 mL of iohexol 0.2% with water divided into three doses (232.5 mL one hour before scanning, 116.25 mL 30 minutes before scanning, and 116.25 mL just before scanning).
CT images were acquired on a 64-slice scanner using 5-mm collimation and reconstruction intervals.
"Both groups had a similar number of diagnoses thought to increase peristalsis, such as hyperthyroidism or GI bleeding," Alhilali said. "The iohexol group was actually more likely than the barium group to have pathology we felt to be more inhibitory to peristalsis, such as gastroparesis...."
Two readers working independently evaluated bowel opacification on a scale of 1 to 3 (with 3 being excellent). The investigators also recorded the most distal portion of the bowel that was opacified in each exam.
According to the results, the two patient groups were comparable in median age (p = 0.76), gender distribution (p = 0.38), location of symptoms (p = 0.89), motility-altering medications received (p = 0.79), and scan preparation time (p = 0.16), the group reported. More iohexol patients had intra-abdominal pathology compared to barium patients (59% and 41%, respectively, p = 0.02).
Overall, the barium group "achieved similar transit to both the distal small bowel (55/59 for barium and 152/169 for iohexol, respectively, p = 0.58) and the colon (25/59 for barium and 84/169 for iohexol, respectively, p = 0.35) when compared to the iohexol group," and radiologists' assessment of image quality scores was also comparable (p = 0.57), Alhilali said. As for cost, iohexol was cheaper per patient.
"Although iohexol costs about 20 times the cost of barium per mL, the ability to significantly dilute iohexol while still retaining the same density means that iohexol for study actually costs about half that of barium," she said. The per-patient cost of barium was $6.30 versus $2.85 for the dilute iohexol.
"Distal bowel opacification was the same in both groups as well as image quality despite a lower cost per patient with iohexol," Alhilali concluded. Moreover, she said, the favorable safety profile of iodinated contrast agents "might suggest an advantage to iohexol for CT exams of the abdomen in the emergency setting." She personally prefers the taste of barium, though patient preference was not evaluated in the study, Alhilali said in response to a question from the audience.
Once again the main study limitation was that the contrast protocols were used on two different patient groups, precluding a direct comparison.
By Eric Barnes
AuntMinnie.com staff writer
January 21, 2007
Related Reading
Study tests low dose ranges for perfusion CT, December 10, 2007
Capsule endoscopy identifies small bowel melanoma metastases, July 9, 2007
CT enterography answers range of small-bowel questions, May 22, 2007
3D reveals what axial images can't in small-bowel CT, November 15, 2006
Distinct CT perfusion parameters help assess HCC, November 29, 2005
Copyright © 2008 AuntMinnie.com




















