Dutch researchers noticed some intriguing results in a recent analysis of data from the ongoing NELSON lung cancer screening trial. They found that malignant nodules, scanned at baseline and follow-up, had higher attenuation overall than benign nodules -- a feature that could potentially aid the management of patients with indeterminate solid pulmonary nodules.
The group cautioned that attenuation of malignant nodules didn't change much between the scans, and suggested that factors other than malignancy may have rendered them brighter. Also, because malignant nodules were larger than benign nodules, they are theoretically less prone to partial-volume effects, which can skew attenuation measurements.
Still, any tool with the potential to shed light on the management of indeterminate lung nodules found at CT screening is worth evaluating, owing to the large number of nodules detected in CT screening programs.
"Because of the rapid development of technology, CT screening views small nodules in 60% to 90% of participants," said Dr. Yingru Zhao from the University of Groningen in Groningen, Netherlands. "Management of these small nodules should focus on the rapid identification of malignant nodules."
Distinguishing malignant from benign nodules is easier said than done noninvasively, however. The most accurate method, biopsy, is invasive, expensive, and risky. In CT images, common predictors of malignancy include larger size, irregular morphology, suspicious nodule consistency, and rapid growth. But no feature is foolproof.
"Benign nodules also grow, and 2D measurements are unreliable in small nodules. So we need additional identification -- maybe density," Zhao said at the 2008 European Congress of Radiology (ECR) in Vienna.
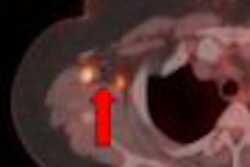
Part-solid nodules have been shown to increase in density during malignant transformation, perhaps owing to invasive growth or response to therapy, Zhao said. This led the study team to hypothesize that the same process might occur in solid parenchymal nodules detected at CT screening of smokers and former smokers for lung cancer.
The group sought to evaluate whether increases in attenuation or changes in morphology, shape, or margin in indeterminate solid pulmonary nodules were associated with malignancy.
The study was part of the NELSON trial, a large-scale experimental screening program led by the University of Utrecht in the Netherlands. In this analysis, principal investigator Dr. Dongmang Xu, PhD; Dr. Mathias Prokop, PhD; Zhao; and colleagues evaluated data from 310 participants who were screened with low-dose CT from 2004 to 2006. All were current or former smokers (95% men, mean age of 63 years).
Data from 16-slice CT scanners were acquired using 1-mm collimation and 0.7-mm reconstruction increments, with the results evaluated by two experienced readers working independently. Mean CT densities were calculated automatically using LungCARE software (Siemens Healthcare, Erlangen, Germany).
"We included indeterminate nodules detected at baseline screening," Zhao said. "Nodules were all solid and purely intraparenchymal, with volume between 50 (mm3) and 500 mm3. Participants underwent follow-up scans at three months and one year."
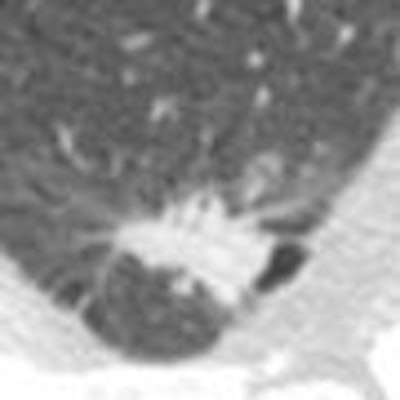
Nodules were classified based on morphology (spherical or nonspherical), shape (round, polygonal or irregular), and margin (smooth, lobulated or spiculated).
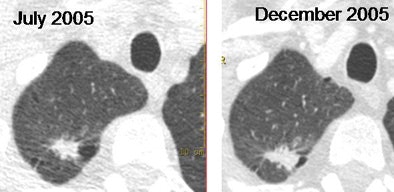 |
| Adenocarcinoma shows rapid growth over six months. Images courtesy of Dr. Mathias Prokop. |
Of the 372 detected nodules, 16 (4%) were malignant and 356 (96%) benign, the team reported. The baseline median CT density was 41.9 HU (range -195.1 to 192.1 HU) for benign nodules and -2.2 HU (range -127.5 to 75.0 HU) for malignant nodules (p = 0.06). The median density change for benign nodules was -0.2 HU (range -93.1 to 175.2 HU) and greater than12.8 HU (range -29.5 to 45.1 HU) for malignant nodules (p < 0.05).
|
Malignant nodules were larger overall, with a median volume of 274.5 mm3 (range 64.4 to 498.0 mm3) compared to 82.8 mm3 (range 50.3 to 491.0 mm3) for benign nodules (p = 0.000). And malignant nodules were more often nonspherical, irregular, lobulated, or spiculated (p < 0.0001), Zhao said.
"Of the 16 malignant nodules, there were eight adenocarcinomas, five squamous cell carcinomas, two large cell carcinomas, and one neuroendocrine carcinoma," she said. "An increase in nodule density at follow-up was found in eight cases."
As for nodule features, a comparison of baseline scans to three-month and one-year follow-up images showed that only one case had changed in margin, and none changed morphology. A Chi-square test revealed no significant change in nodule features, Zhao added.
"Malignant solid nodules tended to have a lower mean density than benign nodules," she said. "This might be caused by the inclusion of air or regressive changes within the tumor, such as necrosis and hemorrhage."
While malignant solid nodules increased in density at follow-up, benign nodules did not show this change, suggesting that the density could be used in screening follow-up recommendations.
"In our study, malignant nodules from the beginning were already larger than benign nodules, and more often had different nodule features, which suggests that malignant features are not acquired in the course of malignant lesions' natural history," Zhao said.
In an e-mail to AuntMinnie.com, study co-author Dr. Mathias Prokop, a professor and chairman of radiology at University Medical Center Utrecht in the Netherlands, cautioned that the results "do not reflect a real increase in the density of malignant nodules, but rather the fact that malignant nodules are on average larger (median 274.5 mm3 versus 82.8 mm3), and are therefore less subject to partial-volume effect." The fact that they grew over the follow-up period makes them even less vulnerable to partial-volume effect, he added.
Compared to benign nodules, malignant nodules were larger at baseline, and more often nonspherical, irregular, lobulated, or spiculated, Zhao concluded. "An increase in nodule attenuation is suggestive of malignancy and requires shorter follow-up or biopsy," she said.
By Eric Barnes
AuntMinnie.com staff writer
April 14, 2008
Related Reading
Canadian CT lung screening tracks asbestos workers, April 3, 2008
CAD provides mixed benefits for DR lung exams, March 8, 2008
Measuring lung nodule growth beyond variability, November 5, 2007
Low-dose CT practical for lung cancer screening, April 30, 2007
Workplace cancers cause 200,000 deaths a year: WHO, April 30, 2007
Copyright © 2008 AuntMinnie.com