The Radiology study was no victory for screening advocates, but then again, the bar for success was high. A new lung cancer model based on 1,520 CT screening subjects found that five years of annual lung cancer screening increased lung cancer detection by an estimated 37% and decreased lung cancer-related deaths by 28%.
However, death from all causes dropped by only 4% over five years of screening, and by 2% over 15 years, calling into question the value of CT screening for smokers and former smokers, according to Dr. Pamela McMahon and colleagues from Harvard Medical School in Boston and the Mayo Clinic in Rochester, MN (Radiology, July 2008, Vol. 248:1, pp. 278-287).
Of course, those who screen for lung cancer can't do much about all-cause mortality. But they can potentially improve their ability to detect lung cancer with diligence and an understanding of the challenges, according to a recent presentation by Dr. Charles White from the University of Maryland in College Park.
"The scope of the problem is considerable," said White at Stanford University's International Symposium on Multidetector-Row CT in Las Vegas. "Missed lung cancer is actually number two after missed breast cancer as a cause of medical litigation." White was referencing a report by the Physician Insurers Association of America that listed missed fractures of the vertebral column in third place.
Contributing factors can be assigned to three broad categories: observer error, lesion characteristics, and technical considerations. "Probably observer error is the most important type," a category that includes scanning errors, satisfaction of search errors, and decision-making errors "like when you read a pulmonary artery as a lung mass," he said.
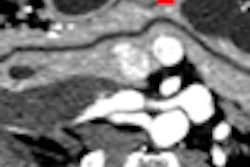
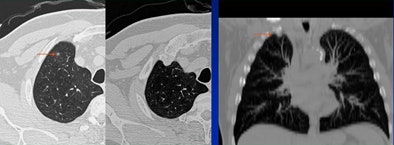
 |
| Decision-making error: Lung mass (arrow, left) was called as a pulmonary artery. All images courtesy of Dr. Charles White. |
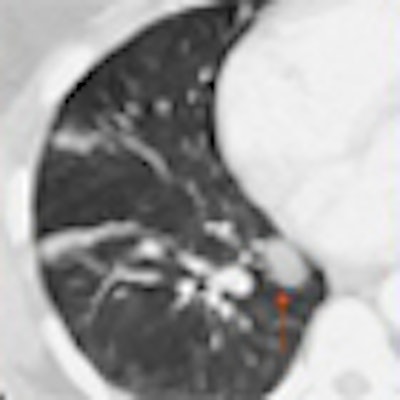
 |
| Satisfaction of search error: The reader found the pacemaker but missed the lung mass behind it. |
"Lesion characteristics themselves may be a pitfall. The smallest detectable lesion is about 4 mm," White said. Studies suggest that the false-negative error rate for 1 cm nodules ranges from 40% to 87%, while the average size of an overlooked lung cancer is considerably larger, at 1.6 mm. "We just completed a study of 100 patients, and [the average missed lesion] was actually about 1.8 cm," he said.
In CT, there are at least three opportunities for diagnostic error: a false-positive diagnosis that occurs when reading a normal structure or nodule as a lung cancer, a false-negative diagnosis that occurs when reading a lung cancer as benign, and a flat-out missed lung cancer that the radiologist fails to visualize.
In false-positive detections, a reader might miscall a normal structure such as crisscrossed blood vessels as a nodule, aka, the classic "internist's tumor," White said. Common errors include miscalling the first costochondral junction, a thickened lateral margin of major fissure, and miscalling loculated pericardial fluid around an inferior pulmonary vein, he said.
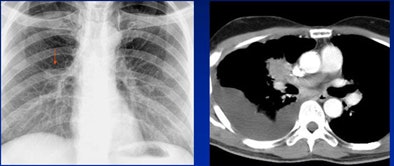
 |
| False-positive: Hypertrophic costochondral junction misread as a lung mass. |
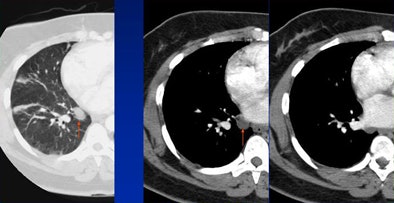 |
| False-positive: Loculated pericardial fluid is often misread as a lung mass. |
Conversely, there are many normal structures that mimic lung nodules, yielding potential false-negative calls, White said. These include granulomas, hamartomas, round pneumonia or atelectasis, arteriovenous malformation, and bronchial atresia.
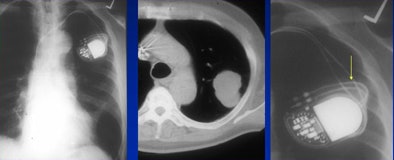
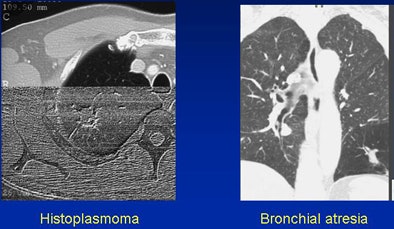 |
| False-negative: Histoplasmoma (left) and air trapping in the setting of atresia (right). |
Lesions with an atypical appearance that may be lung cancers include airspace disease and ground-glass opacities, calcifications, thin-walled cavitation-bulla-associated cancers, cystic lung lesions, and the air-crescent sign.
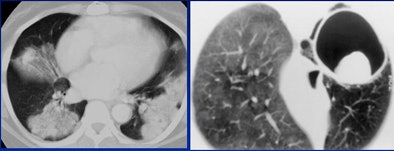 |
| Consolidated bronchoalveolar cell carcinoma represents a classic atypical lesion. |
Small nodules are frequently missed, according to White. The average missed nodule is larger than 1 cm. Swenson and colleagues missed 26% of small lung nodules in a 2002 study. Also, when reading lung data, "don't forget the airways," where many lung cancers hide, White said.
When is a missed lesion malpractice? "This is a complicated topic that goes to medical negligence rules in the U.S.," and it is of course controversial, White said. "Attorneys say any missed cancer is malpractice, and radiologists say it's inevitable."
The literature generally supports the radiologist's view that missed cancers are inevitable, and "the radiology view will eventually prevail," he said. At the same time, "conspicuity is absolutely key" to defending against a missed cancer. Tumors that are large or obvious when seen retrospectively are much harder to defend.
Use computer-aided detection software to cut down on missed nodules. There are several good programs out there, White said.
"This is a daunting and scary topic, and there are a series of medicolegal problems possibly related to observer error, lesion characteristics, and technical errors," White noted. Missed lesions are "unavoidable, but not necessarily malpractice," he said.
By Eric Barnes
AuntMinnie.com staff writer
June 23, 2008
Related Reading
Benefit small from lung cancer screening method, June 11, 2008
CAD helps residents identify lung nodules on DR, May 20, 2008
Ground-glass nodule features on CT reveal malignancy risk, April 29, 2008
CAD shines in detecting large nonsolid pulmonary nodules, February 27, 2008
Evidence for lung cancer screening deemed overstated, December 4, 2007
Copyright © 2008 AuntMinnie.com