Screening subjects in the Netherlands weren't too pleased with the effects of higher laxative doses in a recent virtual colonoscopy (VC or CT colonography) study. Unfortunately, radiologists weren't enamored of the higher laxative doses either.
As Dr. Sebastiaan Jensch and colleagues report in a new study, higher levels of catharsis conferred neither better image quality nor improvement of tagging characteristics on the image data, compared to images from subjects given lower laxative doses.
The 40-patient study from the University of Amsterdam's Academic Medical Center and the Onze Lieve Vrouwe Gasthuis, both in Amsterdam, concluded that minimal doses of laxatives are sufficient to perform VC.
"We hypothesized that a higher level of catharsis would improve image quality but reduce patient acceptance," Jensch and colleagues wrote. "Our objective was to determine the optimal dosage of laxatives for CT colonography with limited bowel preparation with regard to both image quality and patient acceptance."
The group compared image quality and patient acceptance between four regimens with increasing levels of mild catharsis, using bisacodyl and magnesium citrate as laxative agents. The authors noted that although some studies have compared image quality of CT colonography (CTC) with and without laxatives, they believe their study is the first to investigate the effects of different amounts of mild laxatives in CTC (American Journal of Roentgenology, July 2008, Vol. 191:1, pp. 158-167).
The investigators examined 40 subjects with elevated risk of colorectal polyps or cancer (owing to a personal or family history of same) with both VC and conventional colonoscopy. The recruited patients had been scheduled for colonoscopy alone (with a polyethylene glycol prep), adding VC as an additional component of the screening protocol.
The subjects were randomized into one of four groups: Group 1 received 20 mg of bisacodyl orally, group 2 received 30 mg of bisacodyl, group 3 received 20 mg of bisacodyl with 8.2 g of magnesium citrate, and group 4 received 30 mg of bisacodyl in addition to 16.4 g of magnesium citrate. All patients followed a two-day low-fiber diet and ingested diatrizoate meglumine and barium for fecal tagging.
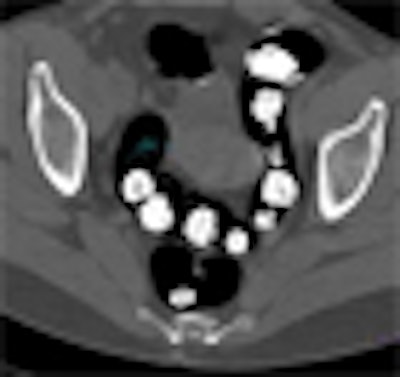
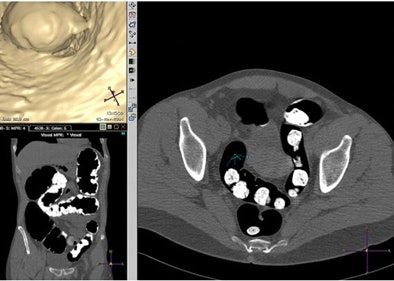 |
| Axial multiplanar reformatted coronal and endoluminal 3D images show subjective evaluation in four different patients with various grades of fecal tagging. Above, in 51-year-old woman with history of colorectal polyps, reviewer evaluated fecal tagging as good. Image republished with permission of the American Roentgen Ray Society. Jensch S, de Vries AH, Pot D, et al. Image quality and patient acceptance of four regimens with different amounts of mild laxatives for CT colonography. AJR. 2008;191(1):158-167. |
Just before scanning, most subjects also received antispasmodics, either scopolamine bromide (Buscopan, Boehringer Ingelheim, Ingelheim, Germany) (n = 22) or 1 mg of glucagon hydrochloride (GlucaGen, Novo Nordisk, Bagsvaerd, Denmark) (n = 17) intravenously. Finally, automated insufflation was administered (ProtoCO2l, E-Z-EM, Lake Success, NY).
VC was performed in the supine and prone positions on a four-slice scanner (Mx8000, Philips Healthcare, Andover, MA) using 120 kV and either 50 mAs or 70 mAs for patients with a circumference greater than 103 cm. Collimation was 4 x 2.5 mm, with a slice thickness of 3.2 mm and reconstruction interval of 1.6 mm.
A single experienced reviewer subjectively scored the quality of images for fecal tagging, amount of residual feces, luminal distension, and image readability on a five- to six-point scale using primary 2D review.
On the day of the exam, patients completed a questionnaire regarding the burden related to diarrhea, abdominal pain, flatulence, and overall burden associated with the VC prep. Five weeks later, they rated their experiences and preferences for either VC or conventional colonoscopy, performed in all patients in four to 30 days (mean, 17 days) after VC.
Image review
Image readability was evaluated as good or excellent in all examinations except for one subject in group 2 (nondiagnostic) and two subjects in group 3 (moderate).
"On a per-patient basis (n = 40), no significant differences were found between groups with regard to image quality," Jensch and colleagues wrote. "All examinations were evaluated as good (diagnostic for lesions ≥ 6 mm) or excellent (diagnostic with no limitations) image readability."
Within each group, a higher degree of tagging homogeneity was significantly associated with better image readability (p < 0.006). Still, no significant differences were observed between groups with regard to mean homogeneity and tagging.
For group 2, poorer bowel distension was associated with decreased image readability (p = 0.002). Group 2 had more feces than group 4 (p = 0.04), a finding mainly attributed to the fact that two of the three patients in the study with relatively low defecation frequency in normal life were placed in group 2, which also included all patients without diarrhea (n = 3). Group 4, which received the highest laxative dose, reported more severe diarrhea than groups 1 and 2 and a higher overall burden from VC than groups 1 and 3 (p < 0.042).
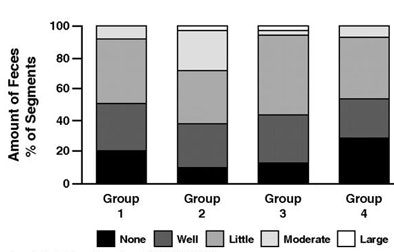 |
| Graphs show subjective image quality scores on per-segment basis. Y-axis shows proportion of segments and x-axis shows preparation groups. Fecal tagging and amount of feces were scored on supine images (for group 1, 66 segments; group 2, 58 segments; group 3, 60 segments; and group 4, 54 segments). Distension and diagnostic readability were scored on supine and prone images (132, 120, 210, and 108 segments, respectively). Group 2 performed significantly poorer regarding amount of residual feces comparison to group 4 (p = 0.04). Image republished with permission of the American Roentgen Ray Society. Jensch S, de Vries AH, Pot D, et al. Image quality and patient acceptance of four regimens with different amounts of mild laxatives for CT colonography. AJR. 2008;191(1):158-167. |
Patient experience
All patients had diarrhea except for three patients in group 2, rated mild by six patients (55%) in group 1, six (60%) in group 2, four (40%) in group 3, and one (11%) in group 4. Diarrhea was significantly more of a burden in group 4 than in groups 1 (p = 0.042) and 2 (p = 0.031) but not compared with group 3 (p = 0.179). Regarding abdominal pain (n = 37) and flatulence (n = 37), no significant differences were found among groups.
One patient in group 4 had severe abdominal pain, and two patients (groups 2 and 4) had moderate abdominal pain. The remaining patients had little (n = 6) or no (n = 28) pain. One patient in group 4 experienced severe flatulence, one patient in group 2 reported a moderate burden, and the other patients experienced little (n = 5) or no (n = 30) flatulence burden.
Burden for the overall bowel preparation was rated as none or mild by all patients (100%) in group 1, nine (90%) in group 2, eight (80%) in group 3, and five (55%) in group 4 -- a significantly higher total burden in group 4 than in groups 1 (p = 0.002) and 3 (p = 0.02). Similarly, most patients experienced no burden or a minimal burden regarding barium intake (32/34), diatrizoate meglumine (36/40), bisacodyl (34/37), or magnesium citrate (9/15) -- and no significant differences were seen between the groups, Jensch and his team wrote.
Regarding the five-week follow-up questionnaire, "Except four patients (one in group 2 and three in group 3), all patients found colonoscopy a more burdensome examination than CTC," the group reported. As for future exams, most patients (30/40) expressed a preference for VC. Two patients expressed no preference, and eight opted for conventional colonoscopy due to direct polypectomy (n = 4), shorter prep time (n = 2), a false-positive VC exam in one case, and without a stated reason in one other case. No significant differences in future exam preferences were seen among the groups.
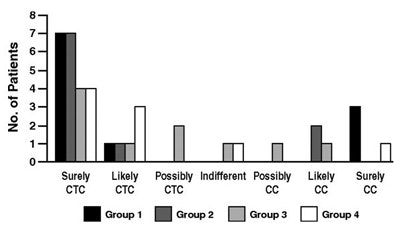 |
| Graph shows patient preference five weeks after colonoscopy. Patients (n = 40) indicated whether they preferred CTC or colonoscopy (CC) as colorectal examination in the future. Most patients (n = 30) preferred CTC. Image republished with permission of the American Roentgen Ray Society. Jensch S, de Vries AH, Pot D, et al. Image quality and patient acceptance of four regimens with different amounts of mild laxatives for CT colonography. AJR. 2008;191(1):158-167. |
"Our results showed good to excellent image readability of CTC examinations (37/40) regardless of the preparation used," the group reported. "Increasing the amounts of laxatives did not lead to a higher attenuation of tagging or to more homogeneous tagging, and subjective image quality did not show significant improvement."
Still, higher laxative doses were significantly associated with a greater burden of diarrhea and the overall bowel preparation. Nevertheless, 35 of 40 patients preferred VC's milder bowel prep compared to the polyethylene glycol prep used for colonoscopy.
The main study limitation pertained to the small cohort size, the researchers noted, with other limitations relating to the placement of specific subjects within the groups. Another potential limitation was the use of only a single reader.
"We conclude that CTC with limited bowel preparation, using barium and ionic iodinated contrast agents for fecal tagging, requires only minimal doses of laxatives -- in our study only 20 mg of bisacodyl -- to obtain good image quality and minimize patient burden," they wrote. "This is important because a mild bowel preparation will undoubtedly increase patient willingness to participate in a screening program."
By Eric Barnes
AuntMinnie.com staff writer
July 16, 2008
Related Reading
Gastroenterologist beats radiologist in dual-prep VC match, June 6, 2008
New low-volume bowel cleansing solution effective, more acceptable, May 9, 2008
VC CAD finds polyps in prepped or unprepped patients, May 6, 2008
Minimal-prep VC may miss more flat lesions, April 17, 2008
Bowel prep with sodium phosphate or PEG pose low risks of renal impairment, January 4, 2008
Copyright © 2008 AuntMinnie.com




















