The presence of coronary artery calcium (CAC) substantially increases the risk of death among the elderly, a risk that increases with rising calcium burden, according to the first large study aimed at assessing the risk of elderly patients with coronary artery disease.
The study in this month's Journal of the American College of Cardiology found that the presence of CAC in the elderly, as in studies of other at-risk populations such as smokers and diabetes patients, "seems to add prognostic significance to risk factors," wrote Dr. Paolo Raggi and colleagues from Emory University in Atlanta; Harbor-UCLA Medical Center in Torrance, CA; and the Tennessee Heart and Vascular Institute in Nashville. "Whether CAC screening has prognostic value when assessing risk in older patients has not been extensively researched" (JACC, July 2008, Vol. 52:1, pp. 17-23).
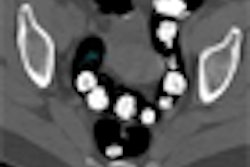
A total of 35,388 asymptomatic patients, including 3,570 individuals 70 years or older, were screened for CAC using electron beam tomography (EBT). A detailed questionnaire was used to record risk factors as categorical variables in all patients, including hypertension (defined as blood pressure > 140/90 mm Hg or treatment with hypertensive agents), hypercholesterolemia (treatment with lipid-lowering drugs), and history of smoking (currently or up to six months before the study).
Electron beam tomography imaging was performed on an Imatron C-150 scanner (GE Healthcare, Chalfont St. Giles, U.K.), which acquired approximately 40 contiguous 3-mm-thick slices at a total radiation dose of 0.6 mSv. Coronary artery calcium scores were calculated using the Agatston method.
Subjects were followed for a mean 5.8 ± 3 years (median 5.0 years, interquartile range: 3.8 to 6.8 years) after scanning, with complete follow-up achieved in all patients.
The researchers found that overall mortality increased with each age decile (p < 0.0001), with a relative hazard of 1.09 (95% confidence interval: 1.08 to 1.10, p < 0.00001). Death rates were higher for men than women, and overall survival was 97.9% (98.2% for women, 97.1% for men). The cumulative survival for various CAC subsets varied by age.
"Survival for a < 40-year-old man and ≥ 80-year-old man with a CAC score ≥ 400 was 88% and 19% (95% and 44% for a woman, p < 0.0001), respectively," the authors wrote. "Among the 20,562 patients with no CAC, annual mortality rates ranged from 0.3% to 2.2% for patients ages 40 to 49 years or ≥ 70 years (p < 0.0001)."
Significantly, scanning for CAC enabled the reclassification of more than 40% of patients 70 years or older, often by excluding risk for patients with CAC less than 400, in those with more than three risk factors. The data show that CAC has a strong prognostic utility even in the elderly; patients without CAC have good outcomes compared to those with high CAC scores, they wrote.
"Several elderly patients had no CAC, and 56% with > 3 risk factors had CAC < 400; hence, they could be reclassified to a lower risk status," Raggi and colleagues wrote. "For younger patients, the relative risk ratios revealed a wide gradient between those with and without CAC, likely because of the fact that baseline risk and comorbidities affect risk in different ways in the young and the elderly."
The study yields important new information that addresses limitations in current assessment methods, according to the authors. For example, both the Framingham risk score and the European SCORE (systematic coronary risk evaluation) methods have upper age limits, and the predictive power of traditional risk factors has been shown to diminish as age increases.
"Because risk factors lose predictive power with advancing age, and the absence of CAC matches a low risk, it may be appropriate to mitigate prevention efforts in elderly patients with no evidence of subclinical atherosclerosis," they wrote. "In Western nations, the elderly are the most rapidly growing segment of the population, imposing increasing costs of care; hence, the need to focus resources on truly necessary interventions exists."
The use of CAC screening in elderly patients may allow for new risk assessment methods as proposed by Grundy and colleagues, which substitute the patient's burden of atherosclerosis for age, they concluded.
By Eric Barnes
AuntMinnie.com staff writer
July 23, 2008
Related Reading
Coronary artery calcium better predictor than carotid IMT of cardiovascular events, July 9, 2008
Coffee inversely associated with coronary calcification in women, May 29, 2008
Coronary calcium still matters, May 26, 2008
Coronary calcium score predicts coronary events in 4 major ethnic groups, March 28, 2008
Coronary artery calcium predicts heart disease events in low-risk women, December 11, 2007
Copyright © 2008 AuntMinnie.com