It's not difficult to miss renal lesions at CT, considering the diminutive size and radiographic subtlety of some lesions. But the right imaging techniques can help ensure that perceptual errors don't get in the way of the diagnosis.
"In renal imaging, the issue remains protocol design -- and it's been the protocols where our successes or failures really happen," said Dr. Elliot Fishman, professor of radiology and oncology and director of diagnostic imaging and body CT at Johns Hopkins Hospital in Baltimore. "The injection rates, the scan parameters, the decision about which phases to choose and how we process the data all become critical."
The protocol design is also a balancing act, he said, because each phase offers its own opportunities and pitfalls, and each additional phase increases the radiation dose.
"We're very conscious of the radiation dose to patients. We're trying to minimize the number of phases we get," Fishman said at Stanford University's 2008 International Symposium on Multidetector-Row CT in May.
Even noncontrast CT has its uses. Ideal for the detection of renal calculi, it is also helpful for defining CT attenuation precontrast versus postcontrast to help determine whether a lesion is a high-density renal cyst. Unlike carcinomas, the appearance of benign cysts tends not to change appreciably following contrast administration.
On the other hand, noncontrast CT scans will miss acute pyelonephritis, as well as vascular pathologies such as arteriovenous malformations (AVMs) and small renal tumors, Fishman said. Without contrast, "small renal tumors that don't change the renal outlines are very easy to miss," he added.
Early-phase imaging has its own advantages. "Thirty seconds [after injection] you're seeing all the vascularity. Ninety-five percent of renal tumors are hypervascular, so you're going to see tumors better at that phase," he said. "But some tumors are not hypervascular and you're going to see these tumors best on late-phase."
In addition, early-phase imaging is best used in combination with other modalities. While it offers significant perfusion information, "if used alone [it] can be a significant source of problems and source errors," he said.
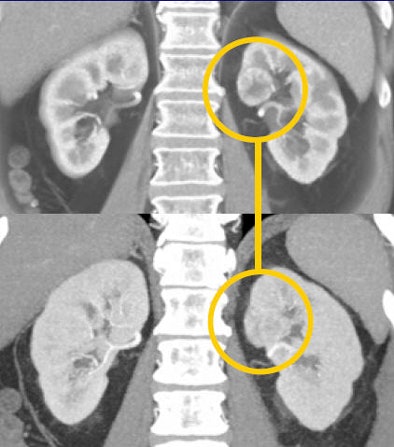
In one patient example, a small hypervascular lesion in the left kidney could not be seen in the early corticomedullary phase, even when the image was viewed in multiple planes, in volume rendering (VR) and maximum-intensity projections (MIPs). It became "a fairly obvious lesion on excretory-phase imaging," Fishman said.
 |
| Subtle renal cell carcinoma not visualized in any plane in the arterial phase (above) becomes fairly obvious in excretory-phase image (below). All images courtesy of Dr. Elliot Fishman. |
 |
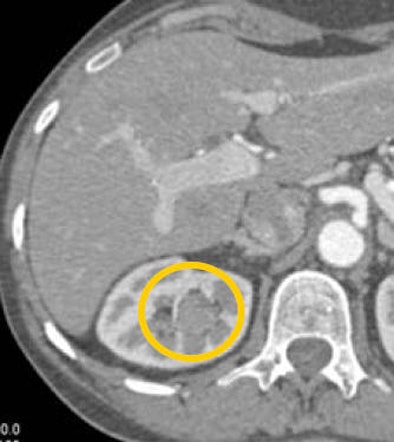
CT images from a patient with transitional cell carcinoma (TCC) were also best appreciated in late-phase imaging. The early-phase data showed slight differential diffusion between the right and left kidneys and a subtle lower-density region in the right kidney. With excretory-phase imaging, the TCC was visible in the axial view and was even more clearly defined in the coronal view.
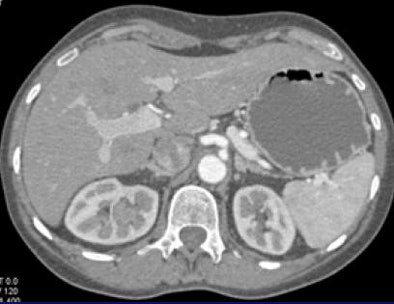 |
| In a patient with TCC, slight perfusion differences can be seen between the right and left kidneys in the arterial phase (above), and a subtle lower-density zone can be appreciated in the right kidney. On excretory-phase imaging, in both the axial view (below) and coronal view (bottom) it becomes an obvious infiltrative tumor. |
 |
 |
In an example of a patient with hematuria, cystography showed a filling defect in the lower pole of the right kidney that appeared to be a soft-tissue mass, and several biopsy attempts were unsuccessful, Fishman said. At CT, excretory-phase imaging seconded the finding, showing what appeared to be a soft-tissue mass. But arterial-phase CT revealed an AVM.
"In this case, late-phase imaging, which typically shows lesions, was misinterpreted, and the patient has a significant hematuria because of the AVM," he said.
In a patient with a subtle 1-cm hypervascular lesion, it was once again the arterial-phase images, combined with a 3D volume-rendered display, that revealed the carcinoma that could not be seen in excretory-phase imaging, Fishman said.
A defining characteristic of renal cysts, on the other hand, is that they tend not to change in appearance after contrast administration, he said.
"Regardless of the phase you choose, from noncontrast to corticomedullary to nephrographic to excretory, every phase has potential pitfalls, which means in designing protocols, a combination of early- and late-phase imaging becomes critical," he said.
The image display format is also important, Fishman said. Findings at the poles of the kidneys tend to be easy to miss on axial images and more readily seen in coronal images, which are especially useful in renal imaging, he said.
 |
| Multiplanar views are important in renal imaging, especially coronal displays (top), which can reveal findings not seen in axial views of the same region (bottom). |
 |
In 3D imaging, a lesion that is invisible on MIPs might be easy to see using a volume-rendering technique.
 |
| A 2-mm renal cell carcinoma not seen in MIP image (bottom) was readily seen in VR image (top). |
Considering the importance of phase acquisition, image display format, and the rendering technique used to view the CT data, optimal lesion detection and classification requires a carefully designed workflow pattern -- from data acquisition to data display, Fishman said.
In a nutshell, the radiologist gets one chance to scan the patient, so if radiation dose didn't matter, the obvious solution would be to do a four-phase study on everyone, Fishman said. But because radiation does matter, "there are two rules: one, you can't do everything, and two, there's no one perfect phase. It's a compromise," Fishman told AuntMinnie.com.
Nevertheless, experience will help the radiologist pick generally two of the best phases for the case at hand, "and more often than not it's a combination of early and late phases," he said.
By Eric Barnes
AuntMinnie.com staff writer
August 28, 2008
Related Reading
Hemodialysis helps prevent NSF in some patients, study finds, August 19, 2008
Clinically significant contrast-induced nephropathy rare, May 14, 2008
Contrast agent osmolality makes no difference in PCI of renal disease patients, April 17, 2008
GFR no better than creatinine for predicting renal failure, December 18, 2007
Sodium bicarbonate best for prevention of contrast-induced nephropathy, October 29, 2007
Copyright © 2008 AuntMinnie.com