SAN FRANCISCO - Choosing cardiac CT angiography (CCTA) first to assess chest pain is more cost-effective than initial stress myocardial perfusion cardiac MR for all but the highest-risk patients, according to a presentation at the Society for Cardiovascular Magnetic Resonance (SCMR) meeting.
The study examined both conservative and aggressive strategies for assessing chest pain using multiple imaging modalities. They found that using CCTA first, followed by cardiac MR if CT found significant disease, saved money and extended the lives of patients better than several other strategies, including that of no imaging tests at all.
The exception was for patients with a high pretest probability of coronary disease, who did better for less money by undergoing MRI first.
"Right around up to a pretest probability of 70%, the sequential approach with CTA as a gatekeeper followed by cardiac MR only if there was significant disease at CCTA was the most cost-effective," said Dr. Steffen Petersen from Barts and the London School of Medicine and Dentistry.
Changing patient management
Management of patients with chest pain changed in 2010 when National Institute for Health and Clinical Excellence (NICE) guidelines were published in the U.K. The new guidelines eliminated ECG from the diagnostic workup of stable chest pain patients suspected of coronary artery disease, and suggested new tests depending on patient risk, Petersen explained.
NICE "suggests identifying patients for pretest probability of significant coronary disease, and for the lower-risk group, 10% to 29%, an anatomical test is suggested based on cardiac CT, and for the intermediate range, 30% to 60%, a functional test is required such as MR," he said.
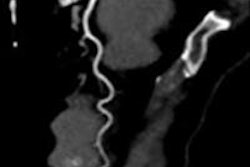
The poor correlation between anatomy and the functional significance of coronary artery stenosis is well-known, but cardiac CT is an excellent test for ruling out significant coronary disease owing to its high sensitivity of 95% to 100% for significant stenosis, Petersen noted. CMR is also highly accurate for diagnosis, with one statistical model assigning it sensitivities of 83% to 91%, with specificities of 81% to 86%.
Petersen, Dr. Tessa Genders, Dr. Francesca Pugliese, and colleagues aimed to determine the comparative effectiveness of CCTA and CMR in the diagnostic workup of patients with stable chest pain.
They developed a Monte Carlo two-level simulation model that modeled diagnostic outcomes in a decision tree, then extrapolated the findings for a lifetime prognosis based on a Markov model, Petersen said.
The cost-effectiveness piece was based on cost data from the U.S., the Netherlands, and the U.K., and were based on clinical practice standards in the respective nations, he said. Along with Barts in London, researchers from Erasmus University Medical Center in Rotterdam, the Netherlands, and the University of California, San Francisco participated in the study.
In the study population used to build the model, 40% turned out not to have coronary disease, 30% had mild coronary disease, 18% had moderate coronary disease, and 12% had severe coronary disease, he said.
5 management strategies
The study considered five management strategies:
- No imaging tests
- CCTA
- CMR
- CCTA + CMR
- Cather-based angiography
Each of the five approaches was modeled separately for both a conservative pathway and an invasive pathway, Petersen explained. Essentially, when following the conservative strategy, patients with mildly positive test results were not referred for angiography, while in the invasive strategy, patients with mildly positive results were referred for invasive angiography.
One scenario started with cardiac MR stress perfusion, for example. If those results were normal, the patient was referred for medical management. But for a severe perfusion defect, the patient was referred to the cath lab for percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG).
Similarly, starting with CCTA, mild stenosis would be referred for medical management, while significant stenosis would lead to the cath lab and a fractional flow reserve (FFR) test to determine the significance of the stenosis.
In the CCTA + CMR strategy, stenosis of 50% or less at CCTA would lead to medical management, while cases of moderate-to-severe disease would be referred to CMR (but not FFR) to determine the need for angiography.
In the catheter-based angiography approach, FFR came first, followed by angiography if positive, and in the no-test scenario, all patients would begin with a referral to medical management.
"We assumed that patients with a false-negative result would present to physicians and then reach the correct diagnosis within a year," Petersen said. "We did also a sensitivity analysis to say, if it's not as fast as one year, let's see what happens if we assume that within three years they get diagnosed in the model."
CT + MRI edges competing strategies
The top patient workup strategies huddled very close to each other on the cost-effectiveness chart. But for patients with a probability of disease of up to 70%, the sequential strategy of using CCTA as a gatekeeper followed by MRI (for positive CCTA) was the most cost-effective overall. Most of the time the invasive approach, in which the patient was sent to the cath lab for a mild perfusion defect, also won out in cost-effectiveness, Petersen said.
With patients with disease probability of more than 70%, CMR alone was usually the most cost-effective approach, "so in almost all patients, cardiac MR had a very important role to play," he said.
"For a 60-year-old-male with a 30% probability of disease, a do-no-tests strategy was cheaper but less effective, whereas in all the other tests, CCTA and CMR, the sequential strategies are fairly close together in effectiveness; they just differ a bit in costs," he said.
For 60-year-old men and women with a disease probability of 30% (and depending on the country analyzed, up to 70% or 90%), the CCTA, CMR, and angiography strategies were very slightly less effective and slightly more expensive than the winning combination.
Quality-adjusted life years (QALYs) were very similar across imaging strategies, and the difference between tests was mainly driven by costs, Petersen said.
A chart presented during the talk showed the most cost-effective strategies added about 11.8 QALYs at a cost of roughly $22,000 to $24,000, based on an annual cost of $1,700 for each patient's statin medications. If the cost of statins were reduced to $100 annually, everyone's therapy became cheaper, yielding the same total additional QALYs at a cost of roughly $13,000 to $14,000.
Moreover, changing the model to sharply reduce the cost of statin drugs didn't alter the hierarchy of cost-effective imaging tests, with CCTA + CMR remaining the most cost-effective choice.
"We also did tests where we changed the CMR sensitivity and specificity to 95% and 90% [respectively], and it didn't change our main finding," he said. Even changing the disutility of statins to 0, that is, modeling the drugs therapy curve to make it effective in every patient, didn't affect the optimal strategy.
All strategies in which CMR was used first cost slightly more than those employing cardiac CT initially, Petersen said. And compared with the conservative CCTA + CMR strategy, the CCTA + CMR invasive strategy was slightly more costly and slightly more effective.
However, changing the time needed for false-negative results to be correctly diagnosed as obstructive disease from one year to three years made CCTA by itself the most cost-effective test, owing to its low cost and great utility as a rule-out test, Petersen said.
"The sequential strategy of CCTA plus or minus CMR was the optimal strategy for both men and women presenting with chest pain and a pretest probability of less than 70% in all three countries," Petersen concluded. "CMR as an invasive strategy is cost-effective if the pretest probability is higher than that, and the optimal strategy is mainly determined by costs."