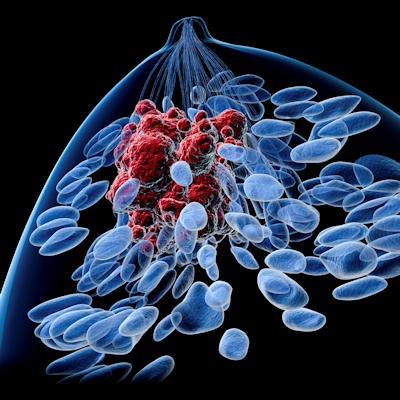
An artificial intelligence (AI) algorithm can expertly detect metastatic lung nodules on chest CT exams in breast cancer patients and aid in risk assessment, according to an April 18 talk at the annual American Roentgen Ray Society (ARRS) meeting.
Researchers from the Medical University of South Carolina (MUSC) found that a commercial deep-learning algorithm yielded performance equivalent to a radiologist in detecting and quantifying lung nodules on CT exams of over 200 breast cancer patients. In addition, they found that the number and size of lung metastases detected by the software strongly predicted disease progression and mortality.
"Specifically, the presence of AI-detected lung metastases impacted survival in patients with estrogen [receptor], progesterone [receptor]-positive breast cancer, as well as HER2-negative tumors," said presenter Dr. Madison Kocher, a third-year radiology resident at MUSC and a 2021 ARRS Resident/Fellow in Radiology awardee.
Radiologists have two roles in the workup of patients who have been newly diagnosed with breast cancer: disease staging of pulmonary metastases on CT, as well as prognostication and treatment guidance, Kocher said.
In patients with metastatic breast cancer, those with only lung involvement have a 32% risk of death within the first year, according to Kocher. As a result, it's important to accurately detect and quantify pulmonary nodules. Unfortunately, this process suffers from significant variability and overall low sensitivity, she said.
Radiologists can also assist in overall prognostication and treatment guidance by quantifying overall nodule volume, enabling a more complete assessment of disease, she said.
To help, the MUSC researchers sought to validate a deep-learning algorithm for detecting lung metastases on CT scans in breast cancer patients. They also incorporated the AI results into a risk-prediction tool that could potentially aid in making treatment and management decisions.
First, they prospectively gathered clinical and imaging data from 226 breast cancer patients aged 25 to 87 who had received a chest CT between January 2014 and January 2019 at their institution. Of these, 168 patients had one or more pulmonary nodules identified by radiologists. The remaining 58 patients did not have any identified pulmonary nodules and served as a control group for the study.
All patients received routine chest CT obtained during breath-hold at end-inspiration and were followed over an average of 2.5 years. To create a reference standard for comparison with the AI results, four radiologists were tasked with reading 25% of the CT exams in a blinded fashion. They measured up to 30 nodules that were 4 mm or larger per patient, calculated the total number of nodules, and noted the location of the greatest diameter of the five largest nodules per patient.
The researchers then applied the AI-Rad Companion Chest CT software (Siemens Healthineers) to the CT exams and assessed its performance in comparison with the radiologists on a per-patient basis for lung metastases and also on a per-nodule basis. Patients were considered to have lung metastases if they had two or more noncalcified solid nodules greater than 6 millimeters or at least one noncalcified solid nodule greater than 10 millimeters.
| Concordance of AI software with radiologist CT interpretations in breast cancer patients | ||
| Per-patient basis | Per-nodule basis | |
| Sensitivity | 95.2% | 97.5% |
| Specificity | 63.9% | 61.2% |
| Positive predictive value | 87.8% | 96.6% |
| Negative predictive value | 83% | 69.6% |
Kocher noted that a previous study had found radiologist sensitivities for pulmonary nodule detection ranged from 51% to 83%. The algorithm can also rapidly assess exams -- an added advantage over the manual process of detecting and measuring lung nodules, she said.
Delving into patient outcomes, the researchers found that the overall number of nodules detected on AI had a weak correlation with overall survival (r = -0.32). In addition, they found that the group of patients with lung metastases were four times more likely to die over the next 2.5 years than those without lung metastases.
The presence of AI-detected lung metastases was negatively associated with survival in estrogen receptor (ER) positive, progesterone receptor (PR) positive cases, as well as HER2-negative cancers.
"This suggests that accurately quantifying the lung metastatic tumor burden is critical in determining an accurate prognosis in [ER, PR-positive] cancer and HER2-negative cancers," she said.
In further results, the researchers found that every 1 mm increase in maximal nodule size increased mortality by 3%. What's more, every additional lung metastasis identified by AI raised mortality by 7%.
The researchers then used the AI results to create classification and regression tree models for assessing risk. These models produced an area under the curve (AUC) of 0.857 for predicting mortality when using clinical, pathological, and image-based characteristics, and an AUC of 0.826 when using only two variables: total number of nodules and maximal nodule size on AI.
Kocher acknowledged the limitations of their study, including its single-center nature.
"A multicenter study of breast cancer patients would allow generalization of our findings to a wider population," she said.