The degree of net water uptake (NWU) on CT imaging in patients who present with large ischemic lesions after stroke can help predict whether endovascular thrombectomy (EVT) will be effective, researchers have reported.
"[Our study] found that the degree of NWU modified the treatment effect of EVT, with higher NWU being associated with reduced EVT efficacy," wrote a team led by Gabriel Broocks, MD, of University Medical Center Hamburg-Eppendorf in Germany. The group's findings were published November 4 in Radiology.
Recent research has shown that supplementing best medical treatment with EVT can improve the functional outcomes of patients with large ischemic lesions. (Best medical treatment may include intravenous blood clot-dissolving drugs or managing blood pressure and glucose.) But for most patients, "prognosis remains poor because a significant injury has already occurred," the group noted, writing that "this has led to a critical clinical challenge: identifying which patients are likely to benefit from EVT."
To this end, the team investigated whether NWU -- identified as infarct hypoattenuation on noncontrast CT -- influences the treatment effect of EVT and whether it could help clinicians determine which patients would respond well to it. The group used data from The Efficacy and Safety of Thrombectomy in Stroke with Extended Lesion and Extended Time Window (TENSION) trial; TENSION enrolled individuals with anterior circulation stroke and an Alberta Stroke Program Early CT (ASPECT) score of 3 to 5 (0 to 4 equals poor prognosis, 5 to 7 equals intermediate prognosis, and 8 to 10 equals good prognosis). The primary outcome of the study was the 90-day modified Rankin scale (mRS) score (a scale of 0 to 6, with 0 equal to no symptoms and 6 equal to death).
Broocks and colleagues' study included 207 patients with a median NWU of 16.4%. Overall, they found that greater NWU was associated with less effective EVT.
They reported the following:
- Higher NWU was an independent predictor of higher mRS scores on day 90, whereas EVT was associated with lower mRS scores.
- There was significant interaction between EVT and NWU (p < 0.002), which suggested "greater treatment efficacy in patients with low NWU," the team wrote.
- EVT in patients with an NWU of less than 15% was associated with better outcomes at three-months post procedure (less than or equal to 3).
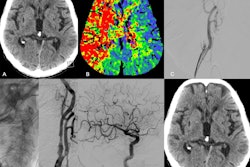
 Axial noncontrast CT (NCCT) images in patients in The Efficacy and Safety of Thrombectomy in Stroke with Extended Lesion and Extended Time Window (TENSION) trial who underwent endovascular thrombectomy with low versus high ischemic lesion attenuation. The two cases highlighting differences in relative hypoattenuation in patients included in the TENSION trial. Patient 1 (upper row) was a 74-year-old female with acute ischemic stroke due to a proximal occlusion of the right middle cerebral artery, NCCT, axial plane; no contrast used. Baseline Alberta Stroke Program Early CT Score (ASPECTS) was 5, with high net water uptake (NWU). Patient 2 (lower row) was a 68-year-old male with acute ischemic stroke due to a proximal occlusion of the right middle cerebral artery; NCCT, axial plane; no contrast used. Baseline ASPECTS was 3, with low NWU. The patient with high NWU (upper row) died despite successful endovascular treatment. The patient with low NWU (lower row) achieved functional independence (modified Rankin scale score of 2). Images and caption courtesy of the RSNA.
Axial noncontrast CT (NCCT) images in patients in The Efficacy and Safety of Thrombectomy in Stroke with Extended Lesion and Extended Time Window (TENSION) trial who underwent endovascular thrombectomy with low versus high ischemic lesion attenuation. The two cases highlighting differences in relative hypoattenuation in patients included in the TENSION trial. Patient 1 (upper row) was a 74-year-old female with acute ischemic stroke due to a proximal occlusion of the right middle cerebral artery, NCCT, axial plane; no contrast used. Baseline Alberta Stroke Program Early CT Score (ASPECTS) was 5, with high net water uptake (NWU). Patient 2 (lower row) was a 68-year-old male with acute ischemic stroke due to a proximal occlusion of the right middle cerebral artery; NCCT, axial plane; no contrast used. Baseline ASPECTS was 3, with low NWU. The patient with high NWU (upper row) died despite successful endovascular treatment. The patient with low NWU (lower row) achieved functional independence (modified Rankin scale score of 2). Images and caption courtesy of the RSNA.
EVT outcomes were better in patients with lower NWU, while in patients with an NWU of at least 15%, EVT plus best medical treatment did not show a functional benefit over best medical treatment alone, according to the researchers.
How these results should be used in clinical practice remains unclear.
"The implications of this analysis can be considered from two perspectives," they concluded. "On one hand, patients with high lesion NWU benefited less from EVT plus best medical treatment than patients with low lesion NWU. This finding could support withholding EVT in this subgroup, particularly in elderly patients with poor prognoses or in stroke centers located in resource-limited settings. On the other hand, this study did not reveal any evidence of additional harm caused by EVT."
The complete study can be found here.