Incomplete smoking history documentation in electronic medical records and limitations of current U.S. Preventive Services Task Force (USPSTF) guidelines appears to result in lung cancer cases being missed on screening, according to research presented at the RSNA meeting.
The study findings highlight "the need for better data capture and more inclusive risk-based screening strategies," said presenter Omar Cespedes-Gomez, MD, of Irvine Medical Center in Orange, CA, who noted that "current USPSTF screening criteria exclude a significant portion of individuals ultimately diagnosed with lung cancer."
Annually, lung cancer causes more than 130,000 deaths in the U.S., more than breast, prostate, and colorectal cancer deaths combined, and 80% to 85% are attributed to smoking, he said. In 2021, the USPSTF released updated lung cancer screening guidelines that lowered the starting age from 55 to 50 and adjusted smoking history from 30 pack years to 20 pack years in an attempt to catch lung cancer earlier and address healthcare inequities among different racial and ethnic groups and between men and women. Screening uptake has increased from 8 million to 14 million adults between 2013 and 2021, he said, but more must be done to address disparities.
"Only 50% of all patients diagnosed with lung cancer would have met any prior screening criteria," he noted. "The 2021 USPSTF criteria, while improved, still lead to disparities, particularly for younger Black patients -- primarily due to pack-year requirements."
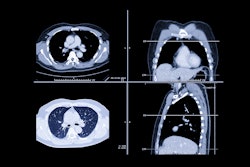
Cespedes-Gomez and colleagues conducted a study that included 1,930 patients between the ages of 50 and 80 who were diagnosed with lung cancer between January 2018 and December 2024. From the medical center's EMR, they culled data such as demographic variables, insurance type, smoking history (pack years, smoking start and stop dates), and evidence of low-dose computed tomography (LDCT) screening within two years prior to diagnosis. They also identified sociodemographic factors associated with missing smoking data and considered predictors of lung cancer screening eligibility.
Of the patients diagnosed with lung cancer, 49% were women, 53% were white, 32% were Asian, 3% were Black, and 12% were of other races and mixed races. Of these, 61% (1,182) had documented smoking history included in their EMR, but only 9.4% of those with complete smoking history who met 2021 USPSTF eligibility criteria for lung cancer screening had undergone it within the preceding two years.
The researchers reported that patients who were male and had Medicare or Medicaid coverage were less likely to have missing smoking data in their EMR (odds ratios, 0.44, 0.61, and 0.6, respectively), while those who were married, Asian, and of mixed/other race were more likely to have missing smoking data (odds ratios, 1.3, 1.6, and 1.46, respectively).
"Women and multiple minority groups face a severe, systematic disadvantage in meeting USPSTF [lung cancer screening] criteria," Cespedes-Gomez said.
He concluded by stressing the need to "prioritize EMR documentation, validate non-pack-year risk models, and implement EMR prompts to increase LDCT identification and completion."