Accurately identifying neurologic manifestations of recreational drug use on CT or MR imaging in emergency department (ED) patients is a key way radiologists contribute to patient care, according to a review published January 8 in RadioGraphics.
"Radiologists interpreting emergency neuroimaging examinations are encouraged to be familiar with the broad spectrum of these findings because prompt recognition and communication are critical for optimal therapeutic management and accurate prognostication in this demographic," wrote a team led by Mariana DeFreitas, MD, of the University of North Carolina School of Medicine in Chapel Hill.
Recreational drug use is a global problem that is increasing in severity, DeFreitas and colleagues explained. They noted that, in the U.S., 7 million to 8 million out of 140 million to 155 million visits to the ED are related to complications from recreational drug use, with common substances including alcohol, cannabinoids, opioids, benzodiazepines, amphetamines, cocaine, and inhalants. Given the use prevalence of these substances, radiologists can "expect to see neuroimaging manifestations of recreational drug use" in the ED.
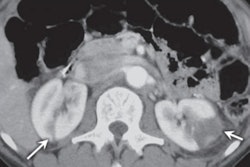
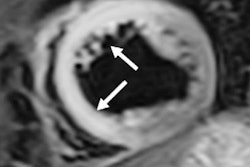
 Acute parenchymal intracranial hemorrhage in a 40-year-old woman with no known medical history who presented to the emergency department with left-sided neurologic deficits and altered mental status. The urine drug screening test result was positive for amphetamines. Axial nonenhanced CT image of the brain shows a right intraparenchymal hemorrhage (arrow) centered in the putamen and the posterior limb of the internal capsule. Image and caption courtesy of RadioGraphics.
Acute parenchymal intracranial hemorrhage in a 40-year-old woman with no known medical history who presented to the emergency department with left-sided neurologic deficits and altered mental status. The urine drug screening test result was positive for amphetamines. Axial nonenhanced CT image of the brain shows a right intraparenchymal hemorrhage (arrow) centered in the putamen and the posterior limb of the internal capsule. Image and caption courtesy of RadioGraphics.
DeFreitas and colleagues offered an overall orientation regarding imaging findings associated with recreational drugs, explaining that these can vary depending on the drug used, the way it is consumed, and the presence of any impurities and stressing that complications may include cerebrovascular structural and functional abnormalities that compromise blood flow to the brain; metabolic conditions due to alcohol, opioid toxic syndromes, and toxic leukoencephalopathies; and bacterial and opportunistic infections and HIV-related diseases.
The team outlined a few key concepts:
- Cerebrovascular complications are the most common types of neurologic insults of recreational drug use, according to the authors.
- "Any pattern of hypoxic-ischemic injury can occur with recreational drug use," DeFreitas and colleagues noted.
- Neurodegeneration resulting in central nervous system atrophy is a "ubiquitous manifestation of the cumulative neurotoxic effects of recreational drugs."
- "Numerous toxic and metabolic conditions related to alcohol use can affect the central nervous system," they wrote. "These can be sequelae of direct neurotoxicity, electrolyte imbalances, vitamin deficiencies, and metabolic dysfunction.
- Intravenous drug use is a "substantial risk factor for bacteremia and endocarditis, which are commonly encountered in clinical practice," they explained. "Risk factors include inoculation with nonsterile techniques or the use of contaminated drug equipment, local soft-tissue trauma and vascular damage, and immunocompromised status."
As recreational drug use is so common, radiologists will "inevitably encounter imaging sequelae … in the emergency setting," according to the team, and "familiarity with these findings is of particularly high value when the patient's medical history is unknown or their neurologic examination is abnormal." Using a framework of cerebrovascular, toxic and metabolic, and infectious abnormalities to assess central nervous system findings of recreational drug use "can help radiologists accurately identify and interpret them," the authors wrote.
"With this approach, the radiologist gains confidence in recognizing drug-related complications and adds value to patient care by contributing to diagnostic accuracy, a critical component of optimal clinical treatment," they concluded.
Access the full review here.