A new, minimally invasive procedure that combines MRI and transurethral ultrasound ablation is effective for treating prostate cancer, according to research presented March 20 at the Society of Interventional Radiology (SIR) meeting in Salt Lake City.
A team led by Steven Raman, MD, of the David Geffen School of Medicine at the University of California, Los Angeles, found that the treatment -- dubbed MRI-guided transurethral ultrasound ablation (TULSA) and performed by interventional radiologists -- proved a viable alternative to surgery or radiation, showing a recovered continence rate of 92% at five-year follow-up.
"This image-guided therapy maximizes our ability to kill cancer cells while minimizing collateral damage to the prostate to achieve the ultimate trifecta in prostate cancer treatment: full local cancer control while maintaining urinary continence and potency," Raman said in a statement released by healthcare public relations firm Reis Group.
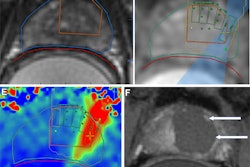
Traditional prostate cancer treatments such as radiation therapy or surgery carry risk of side effects such as urinary incontinence and erectile dysfunction, Raman and colleagues noted. The TULSA procedure consists of the insertion of a catheter-like device into the urethra through the prostate; once the catheter is in place, MRI guides the positioning of 10 therapeutic ultrasound elements into the prostate. Interventional radiologists then use MR thermometry to monitor targeted tissue while heating it to more than 55° and limiting heat to nerves surrounding the prostate at the same time, the investigators explained. TULSA can be performed as an outpatient or inpatient procedure under general or spinal anesthesia and takes two to three hours, the team explained.
In a study that included 115 men enrolled across 13 sites in five countries, all of whom underwent the TULSA procedure, Raman's group found the following:
- Cancer was undetectable on follow-up biopsy by 76% at one year after TULSA with a decrease in median prostate volume by 92% within one year and a decrease in prostate-specific antigen (PSA) from 6.3 ng/ml to 0.63 ng/ml at five years.
- TULSA had a good side-effect profile when compared to surgery or radiation and thermal therapy (the latter being ultrasound-guided high-intensity focused ultrasound [HIFU], or cryotherapy) demonstrating a recovered continence rate of 92% and a preserved erectile function rate of 87% at five-year follow-up.
- Of the study cohort, 25 patients went on to undergo conventional treatment with surgery or radiation because of residual or new tumors, from which the researchers learned that failure of the TULSA procedure was related to calcifications between the urethra and the targeted prostate cancer, prompting "better monitoring of prostate swelling, targeting and misalignment [for] improved detection and management of these preventable errors during the procedure," the group wrote.
"Five-year follow-up demonstrates durable oncologic control, safety, and functional preservation after a single whole-gland TULSA procedure," Raman and colleagues concluded, noting that a randomized controlled trial comparing TULSA with radical prostatectomy is underway.