The highest incidence of nasopharyngeal carcinoma (NPC) is found in southern China, Hong Kong, Singapore, and Taiwan. While currently the accepted imaging modality for post-therapeutic surveillance of NPC, MRI still has difficulty in differentiating postradiation changes from residual or recurrent tumor. As a result, imaging specialists from Taiwan turned to 18F-FDG-PET to test its value in NPC recurrence in patients with questionable MR findings.
For this prospective study, Dr. Ng Shu-Hang and colleagues from Chang Gung Memorial Hospital, Linkou Medical Center in Taoyuan looked at 37 patients who had undergone radiation treatment for NPC between January 2002 and October 2002. The majority of patients (14/37) presented with T4 stage NPC and nodal stage N2 (14/37). MRI was performed 3-4 months after treatment with intensity-modulated radiation therapy and chemotherapy, and every six months for the first two years. The PET study was done 14.1 months after primary treatment (Journal of Nuclear Medicine, October 2004, Vol. 45:10, pp. 1669-1676).
Gadolinium-enhanced MR was performed on a 1.5-tesla unit (Vision, Siemens Medical Solutions, Erlangen, Germany) with a head coil and using a spin-echo technique. The protocol included unenhanced T1-weighted imaging; axial and coronal T2-weighted fat-suppressed FSE imaging; and postcontrast T1-weighted fat-suppressed axial, sagittal, and coronal sequences.
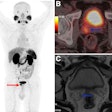
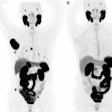
Dual-phase FDG-PET scanning was done on an ECAT Exact HR+ PET system (Siemens and CTI Molecular Imaging, Knoxville, TN) after intravenous injection of 370 MBq of 18F-FDG. Sequential images were obtained from the head to the upper thigh in 56 minutes using a 2D mode. After a three-hour break, a second-phase scan was acquired from neck to head in 25 minutes. Foci of increased FDG uptake were evaluated on a 5-point scale using 0 to represent no abnormal uptake and 4 meaning definitely malignant. Any malignant lesions underwent biopsy.
According to the results, 19 patients had residual or recurrent disease, with five occurring at the primary site, four at nodal sites, and two at distant sites. Using PET, 17 recurrent or residual tumors were detected with 10 confirmed true-negative cases. The sensitivity of PET for recurrent NPC was 91.6%, while the specificity was 76% at the primary site. For recurrence at nodal sites, the sensitivity was 90% and the specificity was 89.9%. At distant sites, PET turned in a sensitivity of 100% and a specificity of 90%. The overall sensitivity at all sites was 89.5% and 55.6%.
"18F-FDG PET provided significant clinical information in 18 of our 37 patients ... revealing unexpected small metastatic lymphadenopathy ... and disclosing distant metastatic foci," the authors wrote. Unfortunately, because of false-positive findings (eight patients) and false-negative findings (two patients), PET did not add information to the MRI results, but did add to the patient's bill, they stated.
PET's greatest strength in NPC patients may be its ability to reveal unexpected tumor recurrence outside the head and neck region, they wrote. But the authors cautioned against substituting FDG-PET imaging for biopsy, particularly during the early post-therapy period (six months), when the majority of false-positives occurred in this study.
"In clinical practice, 18F-FDG PET may be most useful in cases in which MRI findings are questionable but PET findings are true negative, or in which 18F-FDG PET reveals unexpected, true-positive lesions not seen on MRI," they concluded. "However, 18F-FDG PET suffers in specificity for recurrent tumor because it is sensitive to both tumor and inflammation."
By Shalmali Pal
AuntMinnine.com staff writer
November 4, 2004
Related Reading
FDG-PET offers treatment index for postchemo oral cancer, September 30, 2004
Submandibular gland transfer prevents radiation-induced xerostomia, September 15, 2004
Cisplatin plus radiation therapy improves head and neck cancer outcome, May 6, 2004
Atlas of Head and Neck Imaging: The Extracranial Head and Neck, March 13, 2004
Copyright © 2004 AuntMinnie.com