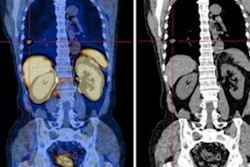
Technetium-99m (Tc-99m) methyl diphosphonate (MDP) bone scans are a potentially viable noninvasive option for diagnosing calciphylaxis, according to a team at the University of Massachusetts in Worcester, MA.
Medical student Morgan Groover and Fnu Nutan, MD, discussed the finding via a literature review of cases that suggest bone scans could play a role over invasive biopsies.
“Skin biopsy is the gold standard for diagnosing calciphylaxis, but it can worsen lesions and confer poorer disease prognosis,” the researchers wrote, in a study published October 23 in JAAD International.
Calciphylaxis – sometimes referred to as “grey scale” – is a rare skin condition most often observed in patients in late stages of kidney disease, with one-year mortality rates greater than 50%, most frequently due to sepsis.
Several reports have considered Tc-99m MDP bone scans as an alternative to skin biopsy in these cases based on uptake of the radiotracer by calcified soft tissue, yet data regarding the sensitivity and specificity of the approach is limited, the authors noted.
The team assessed the potential diagnostic utility of bone scans in calciphylaxis based on a review of the literature. The search yielded 11 case reports and six case series, with 31 patients total. All but one patient had renal disease and most had several other comorbidities, the authors wrote.
“Bone scan supported diagnosis of calciphylaxis in 29 of 31 patients and was 100% sensitive and was 100% specific,” they noted.
Additionally, the search yielded three larger studies from China, U.S., and Canada, which reported the sensitivity of bone scans for diagnosing calciphylaxis to be 62.5%, 89%, and 94.4%. One of the studies had a 97% specificity rate, they wrote.
While promising, the researchers noted that there is no current grading system for radiologist interpretation of bone scans in calciphylaxis. Future studies will focus on standardization of bone scan interpretation guidelines, decreasing inter-reader variability in scan results, and determining sensitivity and specificity, they wrote.
Moreover, clinical correlation and collaboration between the dermatologist and nuclear medicine physician may also still be necessary to reach a diagnosis, they added.
“Given the morbidity and increasing incidence of calciphylaxis and the need for a diagnostic algorithm, the place of bone scan in disease management needs to be better defined,” the authors concluded.
The full article is available here.