PSMA-PET led to management changes in one-third of men receiving salvage radiotherapy for prostate cancer that recurred after radical prostatectomy, according to researchers at the University of California, Los Angeles.
In data from a phase III clinical trial, the investigators found that gallium-68 (Ga-68) PSMA-11 PET initiated major management changes to salvage radiotherapy (RT) planning in 33% of patients – notably, a group for whom the technique was first approved in the U.S. in 2020, wrote lead author Wesley Armstrong, a medical and doctoral student, and colleagues.
“This defines the ‘floor’ of expected changes in management based on existing diagnostic tools,” the group wrote. The study was published January 29 in European Urology.
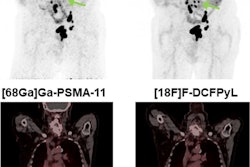
Prostate-specific membrane antigen (PSMA) PET is an effective imaging technique for initial staging and restaging of prostate cancer, with retrospective single-arm studies showing it is more sensitive than conventional imaging, choline-PET, and fluciclovine-PET for detecting recurrent prostate cancer at low PSA levels, the authors explained.
However, the “real-world” clinical impact of incorporating PSMA-PET into salvage RT planning has yet to be determined in randomized prospective imaging trials, they noted.
To that end, the researchers analyzed the use of the technique from a trial they first launched in 2018. This study is an interim analysis on the use of PSMA-PET for managing patients, while the final readout of the primary endpoint -- whether the technique improves outcomes -- is planned for 2025, they noted.
The researchers included a total of 178 with salvage RT plans available who had enrolled in the trial between September 2018 and August 2020 at UCLA and the University of California, San Francisco. They split 76 patients into a control arm and 102 to the PSMA-PET arm; fluciclovine-PET was used in 33 patients in the control arm.
The main management change observed in the PSMA-PET arm was treatment escalation (addition of a radiotherapy field region, androgen deprivation therapy, advanced systemic therapy, or a change to systemic therapy only), which occurred in 37 out of 102 patients (36%) versus nine of 76 (12%) in the control arm.
In addition, about 10% of the PSMA-PET patients received advanced systemic therapy and/or stereotactic body radiation due to extraprostatic disease detection versus 1% in the control arm, the group added.
“PSMA-PET molecular imaging optimizes patient selection for [salvage RT], triggers changes in RT volumes and doses, and the selection for systemic therapy,” they wrote.
Ultimately, while this analysis shows that the technique is effective for improving patient management, it remains speculative whether the changes will result in improved outcomes for patients, the authors noted.
“The final readout of the primary endpoint planned in 2025 may provide evidence on whether these changes result in improved outcomes,” the group concluded.
The full study is available here.