SPECT/CT imaging can help manage patients undergoing radiopharmaceutical therapy (RPT) with Pluvicto for advanced prostate cancer, according to a study published August 8 in the Journal of Nuclear Medicine.
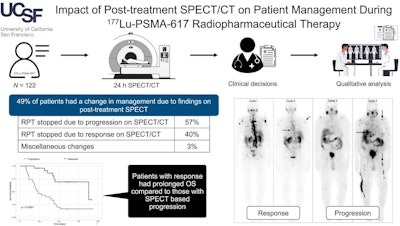
In a retrospective analysis, a group at University of California San Francisco (UCSF) found that qualitative post-treatment SPECT/CT triggered a change in management in 49% of patients, with changes based on progression occurring mostly after two and four cycles of the drug and changes based on response occurring mostly after three and four cycles.
“One of the struggles with [prostate-specific membrane antigen] RPT is how to decide when to stop treatment,” noted lead author Surekha Yadav, MD, and colleagues.
Lutetium-177 (Lu-177) prostate-specific membrane antigen 617 (PSMA-617) RPT (Pluvicto) was approved for adult patients with PSMA-positive metastatic castration-resistant prostate cancer in March 2022.
At UCSF, clinicians perform post-treatment SPECT/CT on all patients undergoing Pluvicto RPT to visualize the distribution of the treatment and to perform quantitative dosimetry, the authors explained. Yet whether SPECT/CT can be used to determine disease progression or response has yet to be delineated, they noted.
To that end, the group assessed the impact of SPECT/CT imaging on 122 patients who had received a minimum of two cycles of Pluvicto and had post-treatment scans after each cycle.
 A graphical abstract of the study.Image courtesy of the Journal of Nuclear Medicine
A graphical abstract of the study.Image courtesy of the Journal of Nuclear Medicine
According to the findings, post-treatment SPECT/CT prompted a change in management in 49% (60/122) of patients. Of these, Pluvicto was stopped early based on post-treatment imaging in 58 (97%): 34 patients had a change based on disease progression and 24 patients had a change based on response, the researchers reported. In two patients (3%), post-treatment imaging led to miscellaneous changes, they added.
Of the 34 patients with changes due to disease progression, most changes occurred after cycle two (47%; 16/34) and cycle four (26%; 9/34). Of the 24 patients with management changes made due to response, most changes occurred after cycle three (38%; 9/24) and cycle four (29%; 7/24), the group noted.
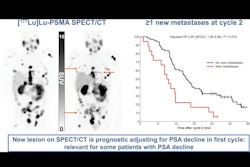
Also, patients who stopped treatment because of response demonstrated improved survival outcomes compared with those who stopped because of progression, the researchers found.
“Integrating posttreatment SPECT/CT into the routine PSMA RPT workflow can streamline personalized patient management by serving as a response marker to RPT,” the group wrote.
Ultimately, imaging tumor response in Pluvicto patients is a particularly difficult issue, with the best approach yet to be determined, the group wrote. CT can be useful to measure morphologic changes, but most patients have bone disease, which is not well evaluated using CT or bone scans, they wrote. Interim PSMA-PET has been proposed, but PET is not as widely available as SPECT and is more expensive, they added.
“Further work aiming at standardization of posttreatment imaging is warranted,” the group concluded.
The full study is available here.