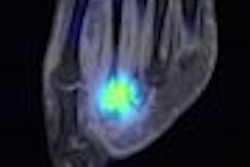
An Australian study is providing evidence that FDG-PET has an important impact on the management of patients with suspected recurrent glioma, and identifies those patients who are more likely to develop progressive disease.
The research comes from the ongoing Australian PET Data Collection Project, which began in October 2001, as a prerequisite for Medicare's further reimbursement of PET in the future. The initiative was scheduled to end last year, but the Australian government extended the deadline to 2009 to gather more information.
"We had to acquire demographic data and specific protocols, which were tied to Medicare indications," said Dr. Michael Fulham, a professor of molecular imaging and nuclear medicine at Royal Prince Alfred Hospital in Camperdown, New South Wales. "The aim of this project is to present data in gliomas and assist in the impact of FDG-PET on the management of patients with a residual structural lesion after prior treatment for glioma and then determine incremental information provided by PET in that context."
Fulham presented the results of the glioma study at the 2008 SNM meeting in New Orleans.
Treatment planning
Three sites contributed information to the study: Royal Prince Alfred Hospital, Sir Charles Gairdner Hospital in Perth, and Austin Hospital in Melbourne. The research included 82 patients (28 women and 54 men, with a median age of 48 years). All but one patient received an MRI prior to PET imaging. Some patients also received a thallium and CT scan. The research began in 2004 and the last follow-up was performed in 2006.
"Referring physicians were asked to specify a pre-PET management plan," Fulham said. "That could include surgery, chemotherapy, radiotherapy, myocardial antibody therapy, or combinations of the above."
The patients also received a PET/CT or PET scan, with the amount of FDG varying per patient depending on the site. There was a standard uptake time of 60 minutes prior to the scan, and no CT contrast was given.
Researchers conducted a follow-up analysis at three, six, and 12 months after the PET scan. At the three-month mark, the study reviewed any changes in patient treatment plans prior to and after PET imaging. After the PET scan was performed, referring doctors were asked to write about the effect of PET/CT on treatment management and complete a post-PET management plan.
Lesion location
"As you would expect, the lesions were fairly evenly distributed across the hemispheres, with slightly more in the right (56%) than the left (44%)," Fulham noted. Other locations included structures in the brain stem. A majority of the lesions were in the frontal (39%) and temporal lobes (26%), with 67% of the lesions classified as high-grade tumors and 33% as low-grade tumors.
As for PET's impact on treatment plans, the study found that PET changed patient management from medium to high impact in 37 patients (45%), which the study described as significant.
In terms of the confirmation of the PET findings, 19 patients ultimately had surgery. There were recurrent high-grade tumors in 10 patients, residual high-grade tumors in four patients, and a combination of high-grade tumors and the effects of treatment and radiation change in five patients.
Among 52 patients, repeat anatomical imaging was performed in the first six months, and anatomical imaging was in agreement with the quantitative PET interpretation in 27% of those cases.
At the three-month mark, 64 patients (78%) received the planned treatment, while 18 patients (22%) did not. Among those 18 cases, 14 patients' treatments were "consistent with the PET results, but there were minor changes in treatment that related to a patient's worsening clinical status or response to initial therapy," Fulham said.
PET's impact
In two cases, the planned therapy was not undertaken because the patients declined treatment. In two other cases, surgery was undertaken, despite the PET findings and concordant confirmation by pathology imaging. "These were patients that the surgeons thought had high-grade tumors," Fulham said, "but the PET said they were not high-grade tumors and the pathology confirmed that."
As for limitations of the study, Fulham noted that there was not pathological confirmation on all PET imaging findings. In addition, two of the contributing sites had been using PET for almost a decade when the trial began, so PET already was included in the diagnostic process. That previous experience with the modality created a "certain confidence in PET findings at those two institutions," he said.
Fulham also noted a potential patient selection bias, because half of the studies came from one site from multiple referring physicians. "This could suggest there was a lack of uniformity expertise in the referring doctors and surgeons, but an alternative explanation is that there were so many referrers that it makes the results more generalized," he said.
The researchers concluded that PET and PET/CT played important roles in changing the management of patient treatment in 45% of the cases. PET and PET/CT also identified through increased metabolism those patients in whom disease was more likely to progress within the next 12 months. In addition, when compared to anatomical imaging, those patients who were least likely to progress in the coming 12 months were more accurately identified.
By Wayne Forrest
AuntMinnie.com staff writer
June 26, 2008
Related Reading
FDG-PET is effective for diagnosing spinal tumors, April 9, 2008
Study shows benefits of very delayed cerebral FDG-PET imaging, December 21, 2007
PET changes oncology management, study shows, July 19, 2007
PET trumps MRI for brain cancer chemo response, July 7, 2006
Dual-tracer PET possible for cerebral gliomas, June 5, 2006
Copyright © 2008 AuntMinnie.com