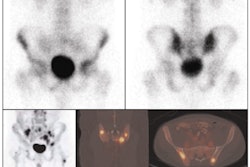
Healthcare providers in the U.S. can save approximately $150 million a year by using FDG-PET/CT, rather than CT, to more accurately identify patients who will benefit from autologous stem cell transplant, also known as a bone marrow transplant.
The calculation comes from a study based at Johns Hopkins Medical Institutions in Baltimore that compared the cost-efficacy of FDG-PET/CT against CT in relapsed diffuse large B-cell lymphoma. Perhaps more significantly, the results show how molecular imaging can contribute positively to healthcare economics.
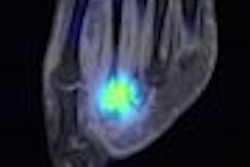
"PET/CT is a superior predictor of clinical outcomes based on patient-specific molecular attributes," said study co-author Dr. Daniel Mollura of Johns Hopkins. "If you can predict what is going to happen to that patient, you can better allocate economic resources so you can achieve clinical benefit as well as economic efficiency."
The study, presented at the 2008 SNM annual meeting, was designed to test the hypothesis that in relapsed diffuse large B-cell lymphoma patients, FDG-PET/CT after salvage chemotherapy more often accurately identifies suboptimally responding patients unlikely to benefit from autologous stem cell transplant.
Data collection
Researchers collected immunological data on diffuse B-cell lymphoma from across the country, cost accounting data on autologous stem cell transplants from Johns Hopkins, reimbursement rates on imaging procedures from the American College of Radiology (ACR), and clinical data from peer-reviewed research, which compared the identification of patients as chemorefractory or chemosensitive with their final outcomes.
Of the 18,957 diffuse large B-cell lymphoma patients analyzed nationwide, the study found that approximately 50% (9,478) of the patients relapse. Of that total, approximately 90% (8,530 patients) are candidates for autologous stem cell transplant (excluding older or comorbid patients), if the relapsed lymphoma is sensitive to chemotherapy.
Approximately 60% of relapsed patients are chemosensitive on CT (5,118 patients), but approximately 20% of those CT chemosensitive cases are chemorefractory based on the FDG-PET/CT (1,023 patients), giving physicians more accurate identification of those patients.
Thus, the study noted, 1,023 "likely nonbeneficial (with increased 5% to 8% mortality) autologous stem cell transplants are performed yearly due to less accurate risk stratification by CT." At an average cost of approximately $150,000 per transplant, $153.5 million would be saved if FDG-PET/CT was used to help determine the risk and potential success, or lack thereof, of a transplant.
Bottom line savings
In addition, based on a cost of $1,200 per CT and approximately $1,400 for FDG-PET/CT, the difference between the two modalities would be $3.9 million annually. "We have this $3.9 million increased cost for the imaging, netting us about $150 million every year in the U.S. from the decreased utilization overall," Mollura said. The individual savings amount to approximately $8,000 per patient.
"An important issue here is whether patients are chemosensitive, meaning by CT criteria a greater than 50% reduction in masses of lymph nodes, so they can get an autologous stem cell transplant," Mollura said. "If they are not chemosensitive, they go into a chemorefractory group, in which case they are not having that proper response to salvage chemotherapy and they cannot get an autologous stem cell transplant."
One reason for the interest in outcomes for autologous stem cell transplant is because the procedure is challenging for patients and has significant morbidity, in terms of immune compromise and infection. "We know there is a 5% to 8% mortality risk, if a patient undergoes autologous stem cell transplant," Mollura said. "Additionally, if you were to transplant a patient who is chemorefractive, greater than 90% will progress by 12 months and the medium patients will progress by five months. So, you really don't want to be transplanting patients who are not likely to respond."
Study limitations
Mollura cited some limitations of the study, including the variability of the cost of an autologous stem cell transplant, which can range from $100,000 to $1 million. The study found the median and average cost clustered around $150,000.
Another consideration is that there are alternative clinical tracks for chemorefractory patients; many undergo conservative treatment, which tends to be inexpensive. Other patients may volunteer for experimental clinical trials. "The point here is that there is no alternative standard of care for these chemorefractory patients," Mollura said.
By Wayne Forrest
AuntMinnie.com staff writer
July 17, 2008
Related Reading
FDG-PET/CT trumps bone scintigraphy for young Hodgkin's lymphoma patients, June 30, 2008
Study evaluates radiation dose, cancer risk for whole-body PET/CT, May 9, 2008
MRI and FDG-PET/CT recommended for advanced breast cancer, April 4, 2008
FDG-PET/CT aids in radiation therapy planning, March 5, 2008
PET/CT moves closer to diagnostic standard of care, March 1, 2008
Copyright © 2008 AuntMinnie.com