First Hill Diagnostic Imaging
Responding to the clinical need for better detection of breast cancer, the number of breast MRI scans is growing by over 40% annually (MRI Census Market Summary Report June 2002, IMV Medical Information Division, Des Plaines, IL). This trend is being driven by the increasing number of women who have a greater-than-average risk of developing breast cancer.
This high-risk group includes women with mammographically dense breasts (sometimes due to hormone replacement therapy); with one or more first-degree relatives with breast cancer; with a personal history of breast cancer or other cancer; or with a recognized genetic mutation (such as the breast cancer gene BRCA1).
The demand for breast MRI is paralleled by the increasing number of outpatient imaging centers dedicated to women’s health issues. These centers offer an integrated approach to the detection, diagnosis, therapy, and long-term follow-up of breast cancer. Mammography, breast ultrasound, freehand and stereotactic biopsy, physical examination of the breast, and consultation are usually offered.
A growing number of these centers offer breast MRI. This exam is usually available through an affiliated imaging facility, although some high-volume women’s imaging centers have acquired their own MRI systems exclusively for breast MR use. In either case, the studies can be read in the women’s health center to best integrate the breast MR findings with the full complement of clinical information.
Although it may be desirable to have the patient’s breast imaging studies read by the same radiologist at the same facility, this approach is often not feasible. The situation has an element of irony: radiologists who are most familiar with breast diseases -- the mammographers -- are in a specialty that has not historically read MRI studies, and the radiologists who are most familiar with body MRI are generally not specially trained in breast diseases.
The environment is changing, however, as mammographers increasingly incorporate breast MRI into their CME courses and fellowship programs, and as body imaging radiologists increasingly collaborate with breast imaging colleagues.
Despite the recent adoption gains, breast MRI studies are still not widely available due to cost, training, time constraints, and integration issues. Computer-aided detection (CAD) can reduce many of these barriers by decreasing processing and analysis costs, standardizing processing functions, and integrating into existing workflows.
Approved uses of breast MRI
The peer-reviewed literature supports the use of breast MRI for selected clinical situations. Clinical applications include high-risk screening, local staging of breast cancer, monitoring response to therapy, and implant imaging (see references below).
CPT codes are available for breast MRI, but there is substantial variation in the coverage offered for this procedure by various third-party payors. The available CPT codes are:
- 76093 Magnetic resonance imaging, breast, without and/or with contrast material(s); unilateral
- 76094 Magnetic resonance imaging, breast, without and/or with contrast material(s); bilateral
A partial list of ICD-9-CM codes that may be eligible for breast MRI are as follows:
|
174.0-174.9 |
Malignant
neoplasm of female breast |
|
175.0-175.9 |
Malignant
neoplasm of male breast |
|
198.2 |
Secondary
malignant neoplasm of the skin of the breast |
|
198.81 |
Secondary
malignant neoplasm of breast |
|
217 |
Benign
neoplasm of breast |
|
233.0 |
Carcinoma
in situ of breast |
|
239.0 |
Neoplasm
of unspecified nature of bone, soft tissue and skin (only when related to the
breast, for example, metastasis) |
|
610.0 |
Benign
mammary dysplasias, solitary cyst of breast |
|
611.0 |
Inflammatory
disease of breast |
|
611.1 |
Hypertrophy
of breast |
|
611.72 |
Lump or
mass in breast |
|
793.8 |
Abnormal
mammogram |
|
996.54 |
Mechanical
complication of breast prosthesis |
Current breast MRI process and analysis
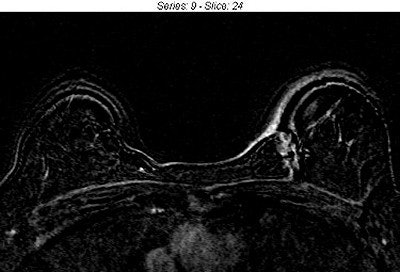
Before discussing the challenges of breast MR imaging, it is necessary to understand how breast MRI studies are currently processed and analyzed. All breast MR imaging, aside from studies performed to assess for implant rupture, includes at least one sequence obtained after administering an intravenous gadolinium-based contrast agent. Although the roles of temporally resolved (dynamic), contrast-enhanced imaging and high spatial resolution imaging are evolving, it is clear that optimal breast MRI requires that both tissue morphology and dynamic enhancement behavior be characterized.
The variation in imaging protocols for breast MR imaging is compounded by the variation in the means used to analyze the images. Some radiologists will tend to focus solely on the images; others will perform time-consuming analyses of the enhancement behavior of various areas of interest. Some will be able to perform ultrasound of the breast following the breast MRI examination to resolve ambiguous findings, while others will not have access to MR-guided breast biopsy or diagnostic ultrasound and will therefore necessarily be forced to accept more ambiguity in the MRI examinations.
Challenges of breast MRI
The processing and analysis of breast MRI is challenging for several reasons.
Large datasets
The dynamic breast MR examination commonly produces 400-800 images before processing. Analysis of the breast MR study involves identifying both areas that show abnormal enhancement and those that have suspicious morphology. Subtraction images can assist in the identification of rapidly enhancing regions, but detailed examination of uptake and washout properties is a cumbersome and time-consuming process in these large datasets.
Artifacts due to patient movement
In addition to the amount of data that must be analyzed, breast MRI is challenging because patient movement can lead to registration errors that produce pseudo-enhancement, mimicking ductal carcinoma in situ (DCIS) and even a suspicious enhancing mass in subtraction images. In some cases, these pseudo-lesions are sent for biopsy, increasing patient anxiety and costs.
 |
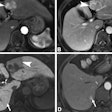
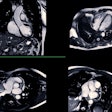
| Breast MRI image before (above) and after (below) registration. Patient had a left lumpectomy for infiltrating ductal carcinoma. Motion artifacts in the image before registration increase the risk that normal structures could be misinterpreted as DCIS and obscure the skin margins. |
 |
| The image after registration more clearly shows the expected normal enhancement around the surgical margin. Misregistration at the skin margin is also greatly reduced.Image courtesy of First Hill Diagnostic Imaging, Seattle, and Confirma, Kirkland, WA. |
Limited patient throughput
Breast MRI workflow can be limited by two factors: low scanner throughput and time to manually process data. A breast MRI study usually requires 30 minutes of scanner time, and, depending on the amount of processing being done, some sites take as much as 15-30 minutes to process a breast MRI study. Processing is sometimes performed at the MR imager console, which can increase scanner and technologist exam time. Limitations in throughput create an economic barrier for many imaging clinics.
Limited standards
Variability in imaging protocols, reader expertise, and technical quality are all factors contributing to the lack of standardization and quality control in breast MR imaging. Breast MRI currently involves non-standardized techniques and terminology. Radiologists are using different doses of gadolinium injected at different time points, different criteria to determine malignancy, different scanning techniques and protocols, different breast coils, and different MRI manufacturers. Technologists also have varying levels of experience with the studies. This lack of standards is one of the reasons cited for the difficulty that breast MRI has experienced in gaining widespread adoption.
Concerns over professional liability
The high profile of the ‘mammographic miss’ in professional negligence litigation may, on an anecdotal basis, decrease the enthusiasm of radiologists trying to decide whether to offer breast MRI (Berlin, L., "Malpractice Issues in Radiology," American Journal of Roentgenology, April 2002, Vol. 178:4, pp. 809-815).
Radiologists may hesitate to adopt breast MRI through the perception that a breast MRI miss will be more likely to lead to litigation than will a miss on a common MRI examination such as MRI of the knee.
How CAD for MRI works
CAD for breast MRI is based on different technology than CAD for mammography. CAD for mammography correlates malignant disease with certain types of calcifications and morphological patterns. The computer analyzes the entire mammogram, looking for suspicious areas and highlighting these areas with markers.
CAD for breast MRI works because malignant disease tends to take up MRI contrast agent at a higher rate than surrounding tissue. This is due to tumor angiogenesis. The computer checks the entire MRI volume, looking for suspicious areas and highlighting these areas with markers. Further, it has been shown that specific patterns of enhancement (enhancement curve types) can add to the accuracy of breast MRI. CAD for breast MRI characterizes the type of enhancement, allowing the radiologist to rapidly consider the curve type in the diagnostic decision (Kuhl, C.K., "Dynamic Breast MR Imaging: Are Signal Intensity Time Course Data Useful for Differential Diagnosis of Enhancing Lesions?," Radiology, April 1999, Vol. 211:1 pp. 101-110).
Another significant difference between CAD for mammography and CAD for MRI is the potential for eliminating many pseudo-enhancements that can be introduced by reading the images conventionally. This means CAD for MRI has the potential of boosting specificity, as well as sensitivity.
Finally, CAD for breast MRI processes studies automatically according to the facility's predetermined configurations. Neither the radiologist nor the technologist need spend any time processing or reprocessing a study -- studies are ready for radiologist analysis shortly after the patient has been imaged.
CAD for MRI in clinical practice
MRI-CAD fits easily into clinical workflow, and there are two approaches to its integration: as a stand-alone workstation or as a network service that is read on a PACS or other available workstation. CAD is set up to receive breast MRI studies from the imager, then automatically process those studies according to predetermined settings.
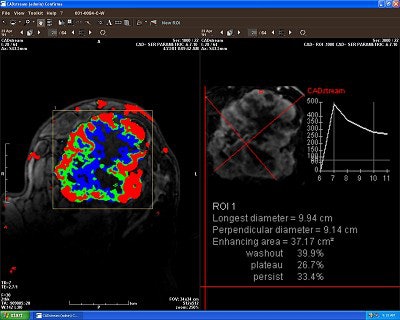
The stand-alone workstation provides processing as well as viewing capabilities. Its color monitor allows the user to view angiogenesis maps and related features. (Figure 2) From this workstation, the user can then archive studies at a PACS or other archive location they are currently using. The network service version of CAD-MRI also automatically detects breast MRI studies leaving the imager, processes the studies, and sends them automatically to a PACS or other workstation. In this scenario, it is preferable that the PACS or workstation monitor have color capability.
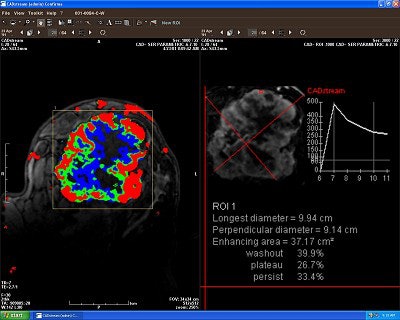 |
| Breast MRI color angiogenesis map (left) and region-of-interest study (right). Image courtesy of First Hill Diagnostic Imaging and Confirma. |
The power of CAD
CAD is positioned to further increase the adoption of breast MRI by decreasing processing times and assisting radiologists with analysis. Consider the following advantages.
Increase patient throughput -- A CAD system automatically processes images according to the site’s or physician’s preferences, freeing the technologist and radiologist from having to process or calculate curves manually. Without a CAD system, it can take up to 30 minutes to process each breast MRI study, depending on the thoroughness of the evaluation. With automatic processing, the next patient can be scanned immediately.
Increase radiologist efficiency -- CAD can enhance analysis of breast MRI studies by pre-processing data into desired outputs. In addition, CAD highlights areas of interest within the large number of data series and provides immediate, detailed information (enhancing area characteristics, diameters, most-enhancing area) within the region of interest on any lesion that the physician wishes to explore thoroughly.
Decrease patient movement-related findings -- A CAD system should take into account patient movement and correct for artifacts generated by patient movement.
Potential to improve the accuracy of breast MRI -- The capability of CAD to improve the accuracy of breast MR image interpretation has not been shown, but is the subject of current clinical research. Given the history of CAD devices for other imaging applications, it seems reasonable to speculate that such improvement is possible, particularly when the system is used to assist less experienced readers.
Provide quality control -- Standardized image processing by CAD promotes reproducibility, consistency, and accuracy. For example, parameters such as contrast uptake and washout can be preset to a level predetermined by the radiologist. In another example, CAD can alert the technologist to excessive patient movement during the scan.
Enhance communication -- CAD can standardize reporting, providing consistency within and between group practices and referring physicians. The visual information provided by a CAD system also allows for enhanced communication between radiologists, referring physicians, and patients.
With an estimated 8.5 million women at high risk of breast cancer in the U.S. in 2001, and recent studies that continue to support the use of breast MRI for high-risk screening and staging, the number of breast MRI procedures is expected to grow rapidly over the next five years. CAD will play a vital role in the proliferation of breast MRI from a specialized diagnostic tool to a common modality for women’s imaging.
By Dr. Justin Smith, RACAuntMinnie.com contributing writer
June 6, 2003
Dr. Justin Smith is board-certified in both nuclear medicine and diagnostic radiology. He is an affiliate investigator with the Fred Hutchinson Cancer Research Center, Seattle, and a medical advisor to Confirma. Smith has practiced at First Hill Diagnostic Imaging in Seattle since 1989, where he specializes in the use of MRI for evaluating cancer.
Related Reading
Confirma adds breast CAD installs, April 24, 2003
Confirma inks research deal with UCSD, April 3, 2003
High breast cancer risk may warrant MR screening rather than mammography, May 7, 2003
Breast cancer in younger women calls for flexibility in imaging, May 2, 2003
Tips and techniques make MRI feasible for breast centers, March 20, 2003
Copyright © 2003 AuntMinnie.com